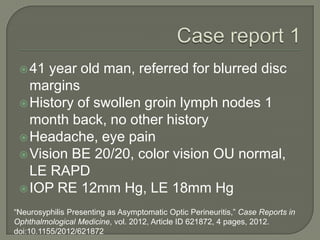
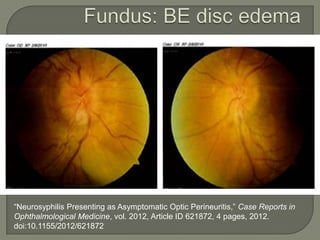
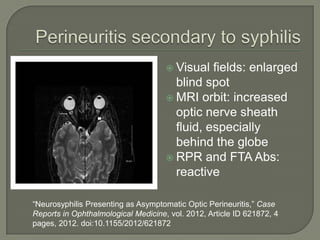
1. A 41-year-old man presented with blurred disc margins and was found to have reactive syphilis serology, indicating neurosyphilis presenting as asymptomatic optic perineuritis.
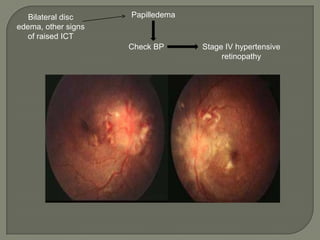
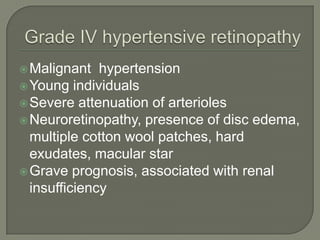
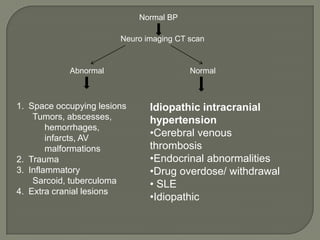
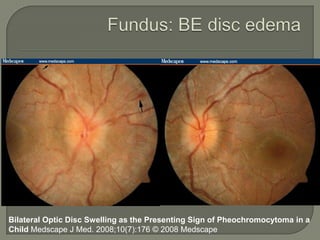
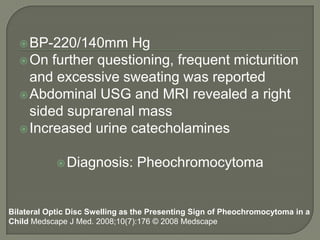
2. A 9-year-old boy presented with intermittent headaches and abdominal pain and was found to have bilateral optic disc swelling and markedly elevated blood pressure, leading to the diagnosis of a pheochromocytoma.
3. In both cases, the optic disc swelling was an unusual presenting sign that led to the diagnosis of an underlying systemic condition.