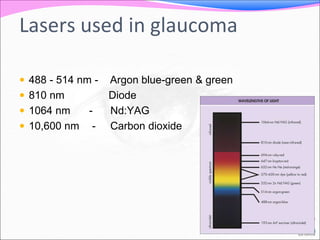
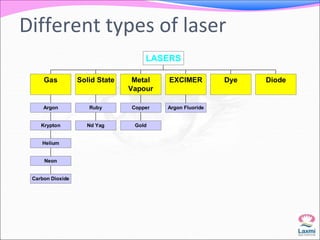
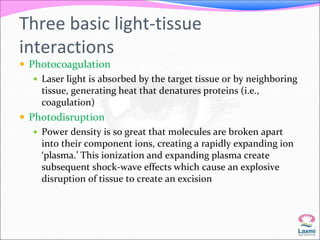
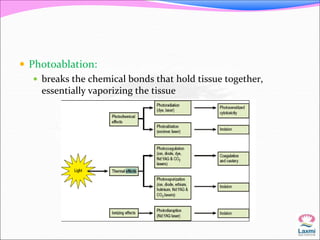
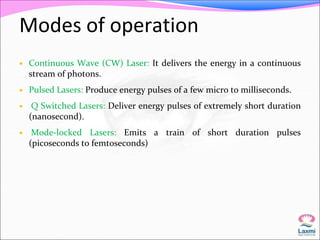
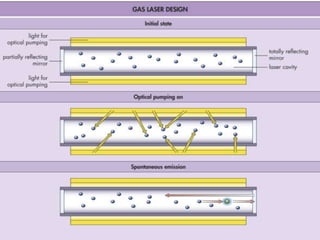
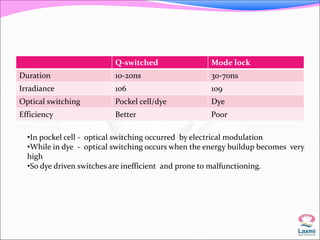
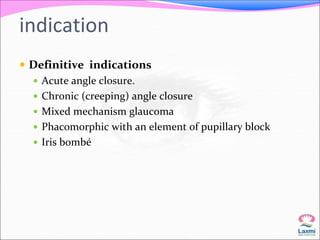
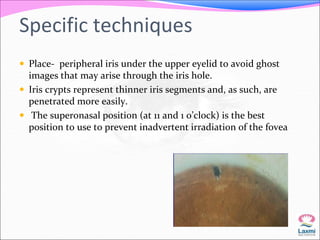
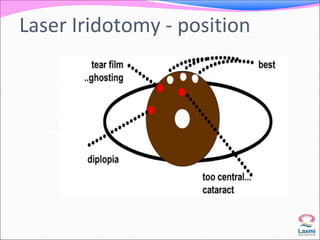
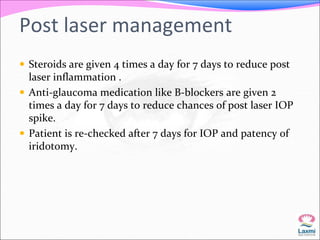
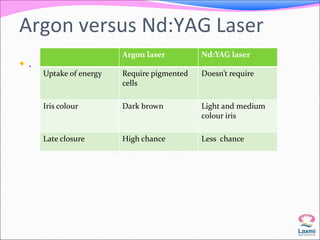
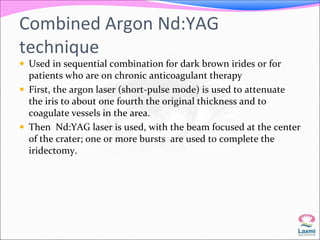
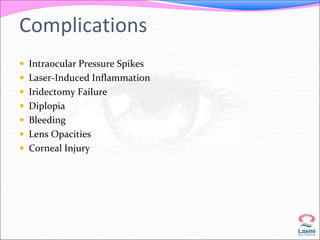
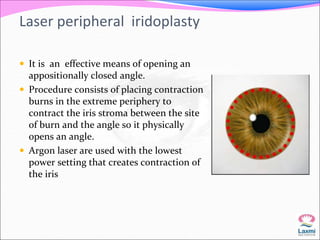
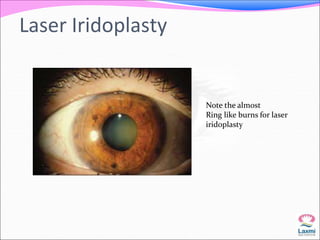
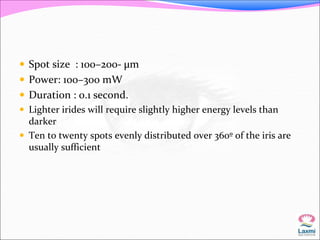
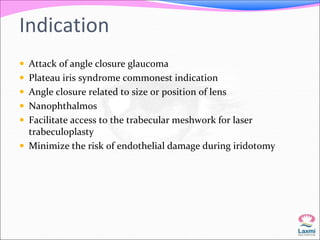
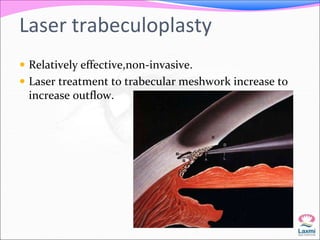
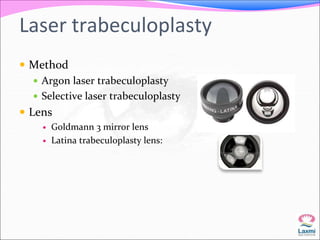
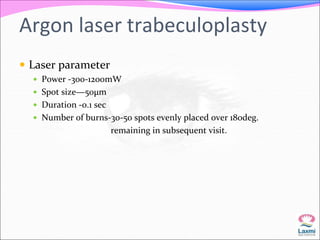
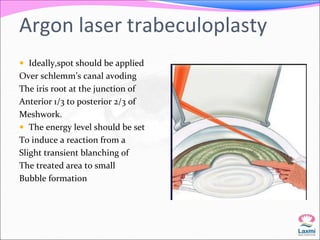
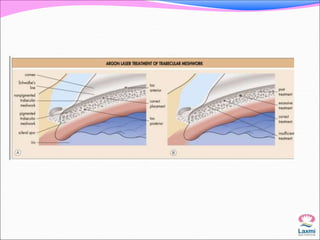
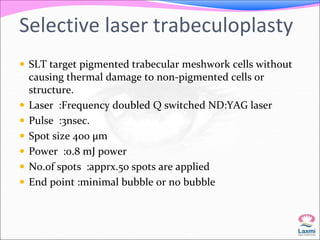
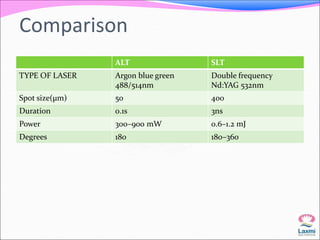
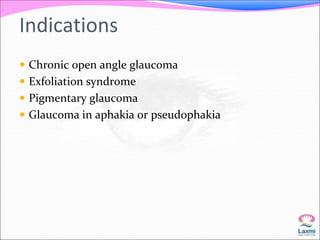
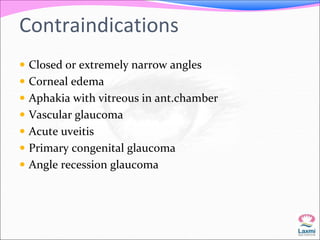
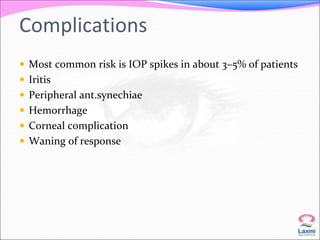
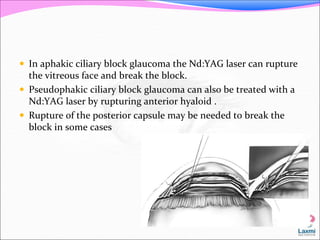
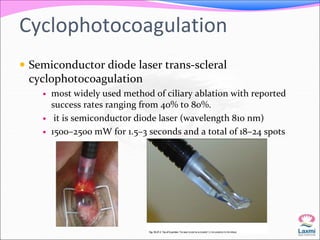
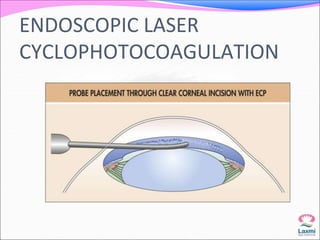
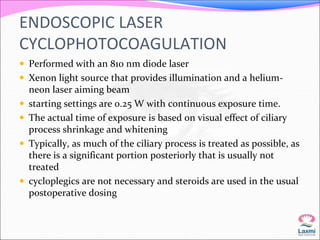
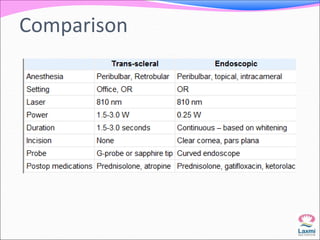
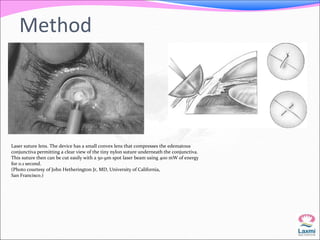
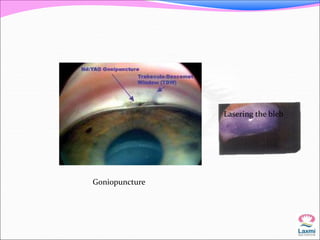
This document discusses the use of lasers in the treatment of glaucoma. It begins by introducing different types of lasers used, including Nd:YAG lasers. It then covers specific laser procedures for glaucoma such as laser iridotomy to relieve pupillary block, laser iridoplasty to modify the iris, and laser trabeculoplasty to increase outflow. It compares argon laser trabeculoplasty to selective laser trabeculoplasty. The document also discusses laser techniques for angle closure glaucoma, post-operative treatment, and cyclophotocoagulation to reduce aqueous production. Throughout, it provides details on laser parameters and outcomes of these procedures.