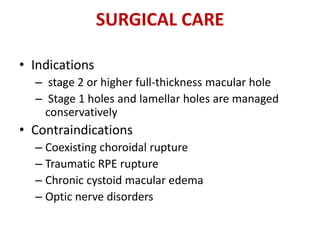
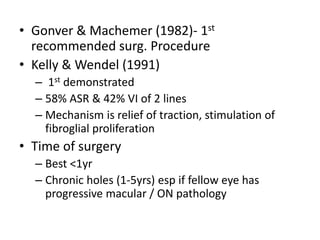
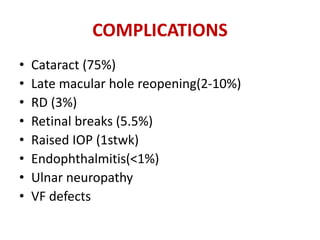
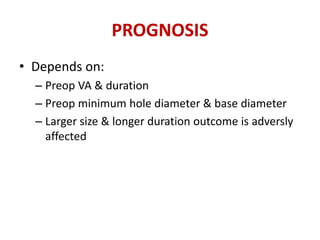
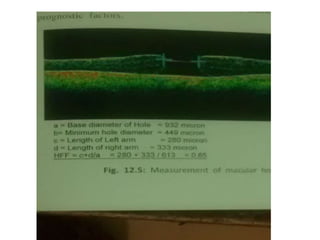
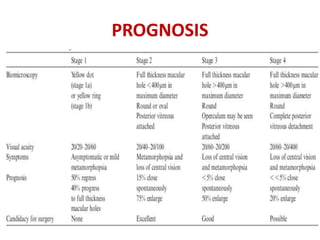
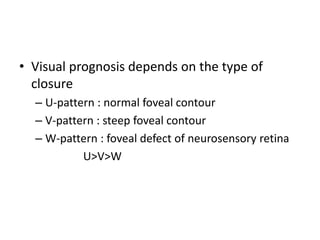
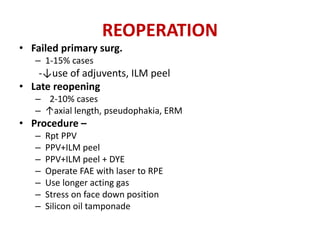
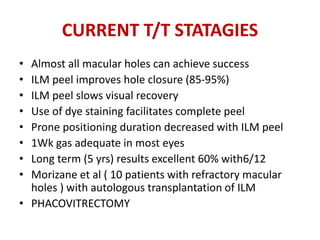
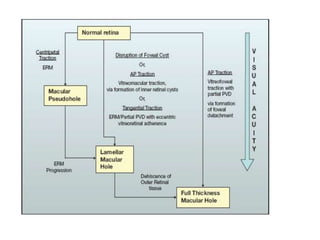
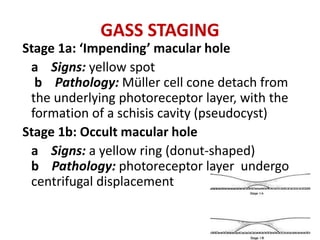
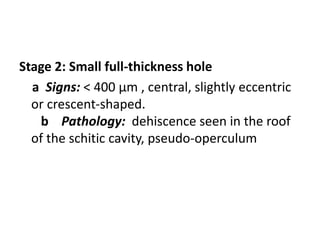
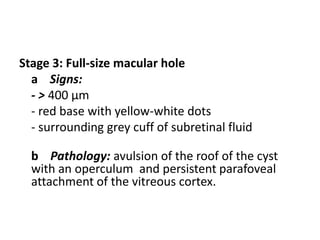
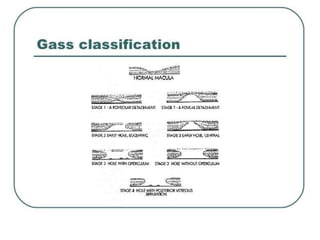
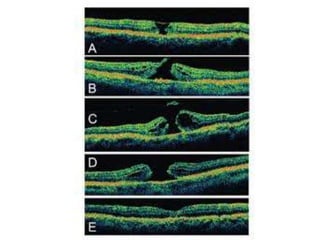
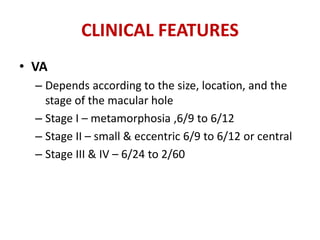
Macular hole is a defect in the macula involving its full thickness. It was first described in 1869. Idiopathic macular holes are the most common type and affect people over age 55. Staging of macular holes ranges from stage 1 to 4 based on size and pathology. Symptoms include decreased vision and metamorphopsia. Diagnosis involves examination, OCT, and sometimes FA. Treatment is usually vitrectomy surgery for stages 2-4 to relieve traction on the macula. Prognosis depends on pre-op vision and hole size/duration, with most patients gaining vision after surgery.
![MANAGEMENT
• NO MEDICAL t/t
• Autologous plasmin
– Idiopathic and traumatic macular holes
– Intravitreal injection of plasmin
– October 2012, ocriplasmin (Jetrea) was approved by
the USFDA for the treatment of vitreomacular
adhesion
– Recombinant proteolytic enzyme
– MIVI-TRUST study group
– Activity against fibronectin and laminin
– Randomized, double-blind study, 652 eyes with
vitreomacular adhesion were treated with an
intravitreal injection of ocriplasmin
– 40.6% of treated eyes compared to 10.6% in the
placebo group ]](https://image.slidesharecdn.com/macularhole-160806130343/85/Macular-hole-24-320.jpg)