This document provides an overview of common errors of refraction, including emmetropia, ametropia, hypermetropia, myopia, and astigmatism. It defines each condition and discusses their etiology, classification, signs and symptoms, investigations, and management approaches. For each error of refraction, the document describes optical and surgical treatment options as well as important considerations for treatment in children versus adults. Overall, the document serves as a comprehensive guide to understanding and managing different types of refractive errors.

























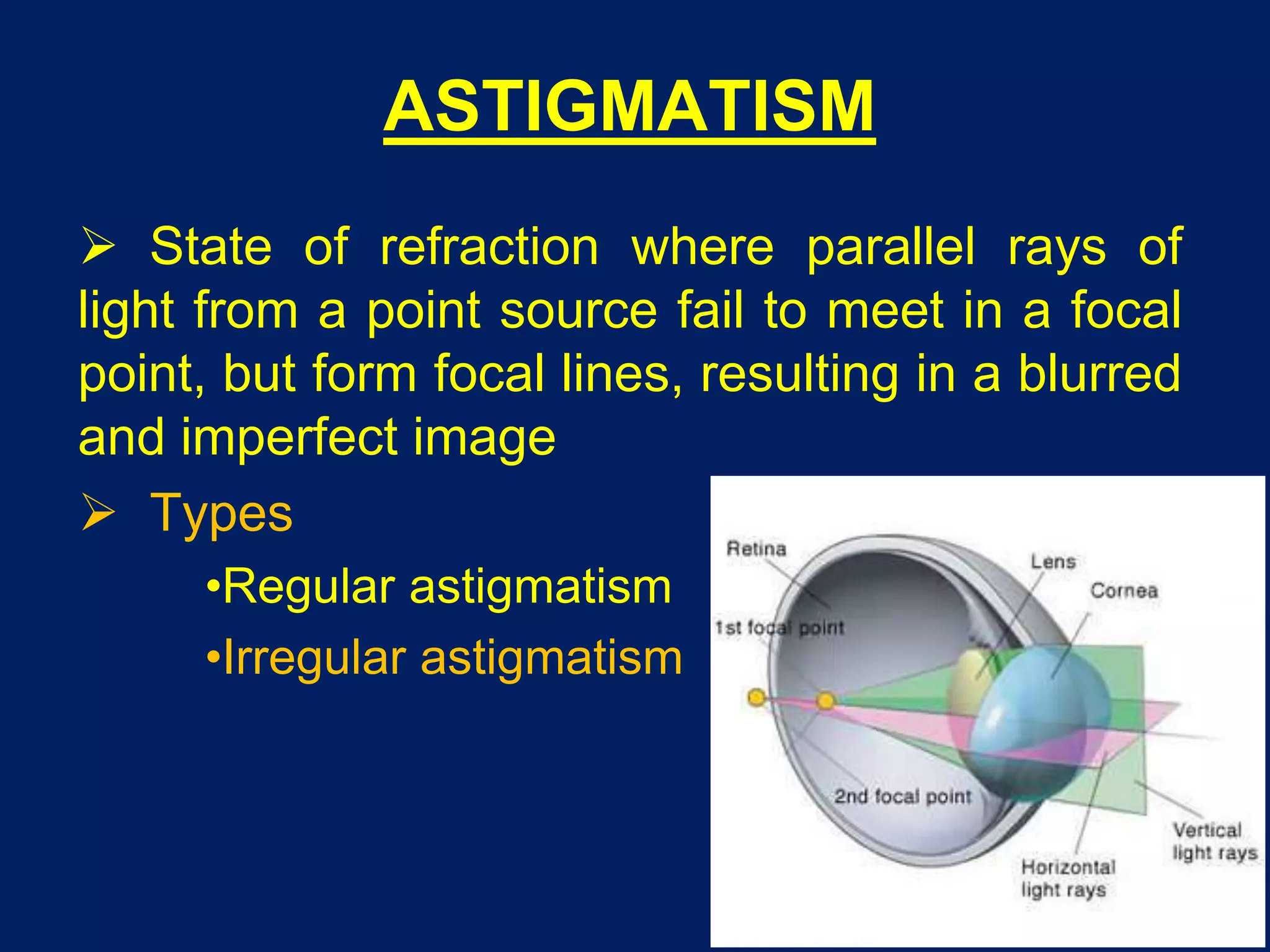


![ETIOLOGY
Corneal astigmatism - curvatural [common]
Lenticular is rare. It may be:
• Curvatural - lenticonus
• Positional - tilting or oblique placement
of lens, subluxation
Retinal - oblique placement of macula [rare]](https://image.slidesharecdn.com/errorsofrefraction-200824062323/75/Errors-of-refraction-44-2048.jpg)