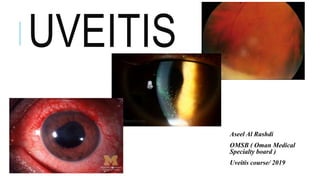
This document provides an overview of uveitis, including:
- The anatomy of the uveal tract and classifications of uveitis based on anatomy, clinical course, etiology, and histology.
- The epidemiology, clinical presentation, signs and symptoms, and common causes of the three main types of uveitis - anterior, intermediate, and posterior uveitis.
- Guidelines for taking a thorough history and performing an examination of a uveitis patient.
- A case example is presented of a patient with bilateral uveitis.