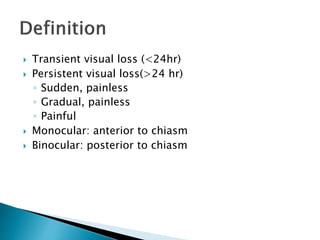
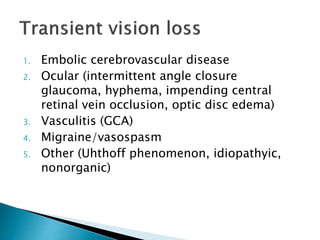
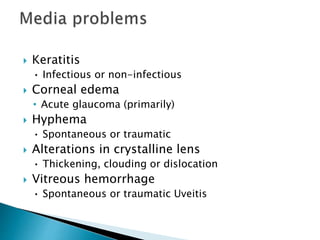
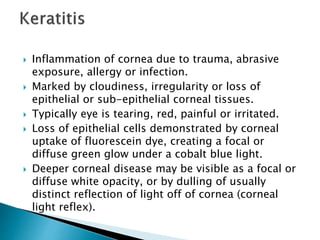
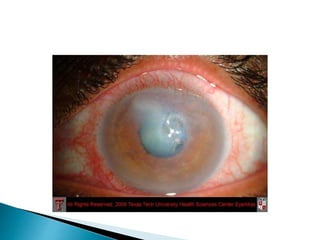
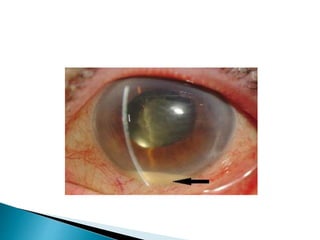
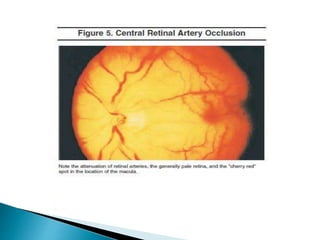
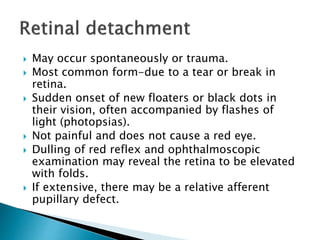
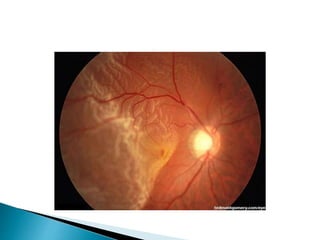
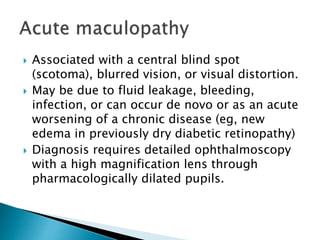
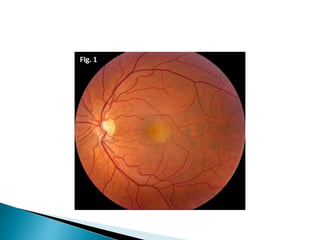
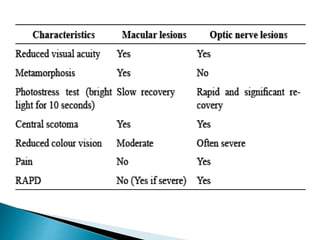
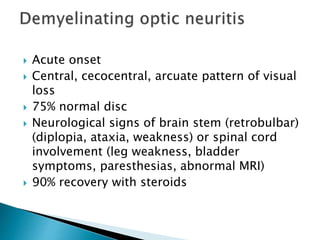
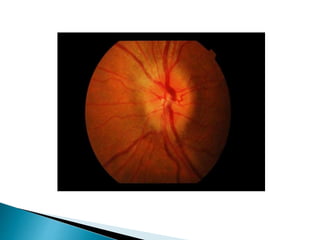
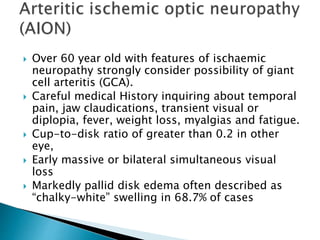
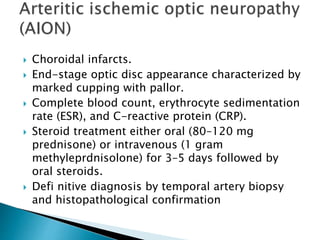
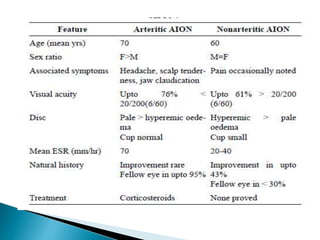
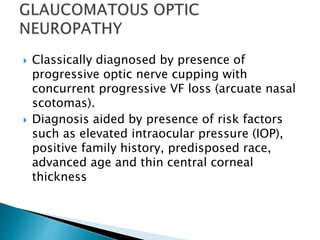
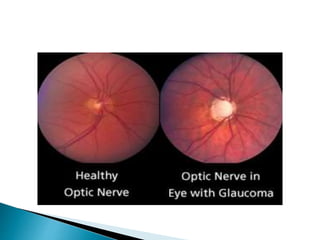
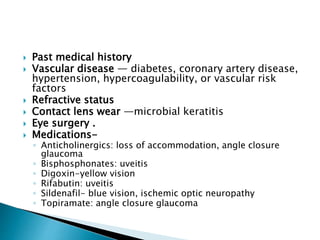
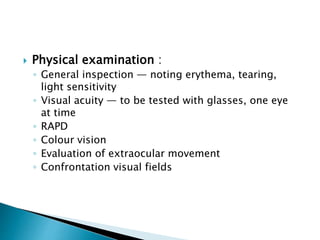
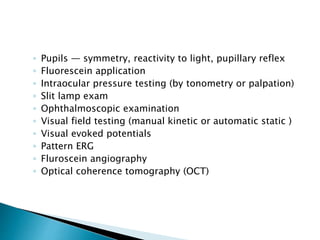
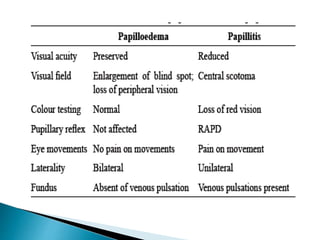
This document discusses various causes of visual loss including transient or persistent visual loss, monocular or binocular visual loss, and various pathologies affecting the media, retina, or neural visual pathway. Specific conditions covered include cerebrovascular disease, ocular issues, vasculitis, migraine, corneal keratitis, corneal edema, hyphema, crystalline lens abnormalities, vitreous hemorrhage, uveitis, retinal vascular occlusions, retinal detachment, acute maculopathy, optic neuritis, giant cell arteritis, malignancy infiltration, and dominant optic neuropathy. Diagnostic criteria and characteristics are provided for many of these conditions.