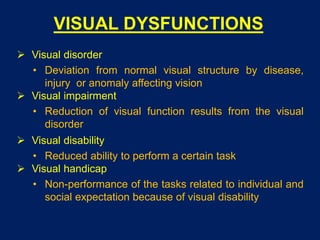
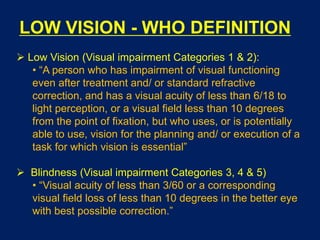
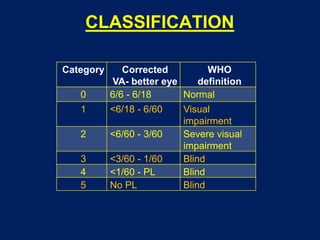
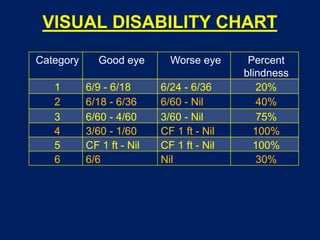
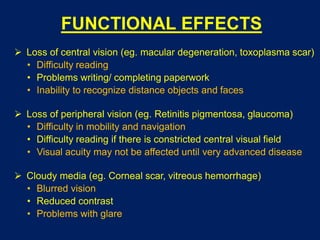
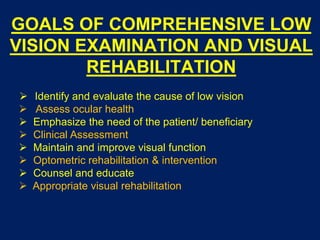
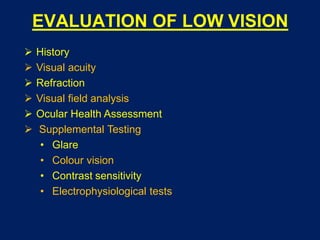
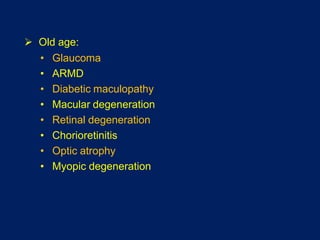
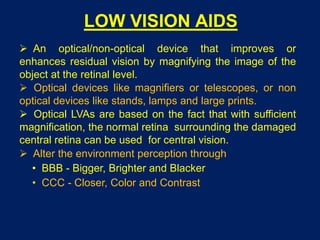
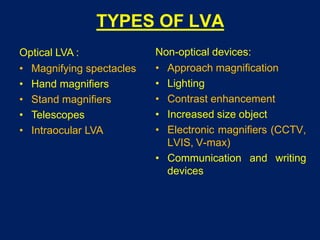
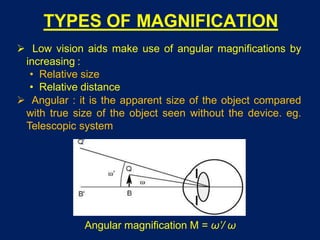
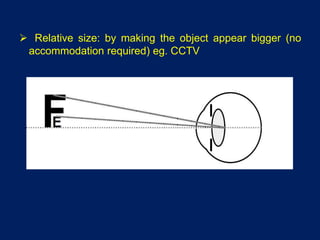
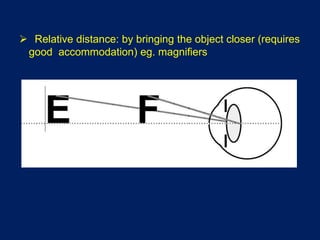
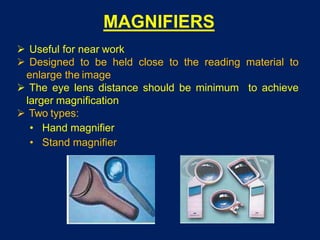
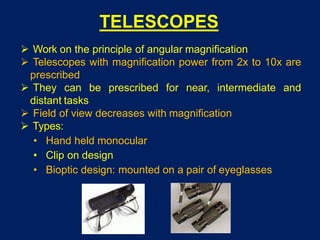
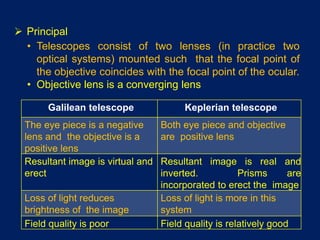
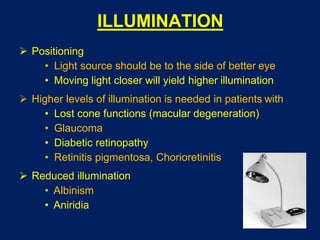
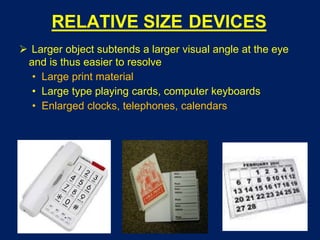
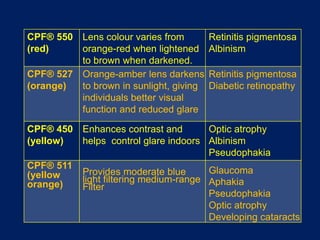
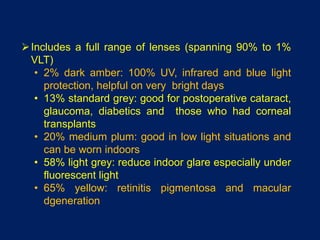
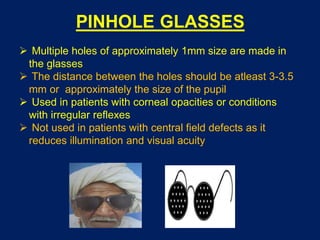
This document discusses low vision aids and their use for people with visual impairments. It defines low vision according to the WHO and describes common causes of visual dysfunction like macular degeneration and glaucoma. The goals of low vision rehabilitation are to maintain and improve visual function through clinical assessment and optometric intervention. Low vision aids can be optical devices like magnifying glasses, telescopes, or non-optical devices that alter lighting, contrast and size of objects. Common optical devices discussed include magnifying spectacles, hand magnifiers, stand magnifiers, and telescopes.