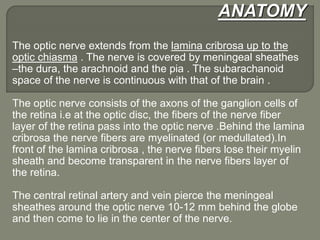
This document discusses optic neuritis, including its anatomy, classification, clinical presentation, diagnostic evaluation, and treatment. Some key points:
- Optic neuritis is inflammation of the optic nerve that can occur in any part of its course from the eye to the brain.
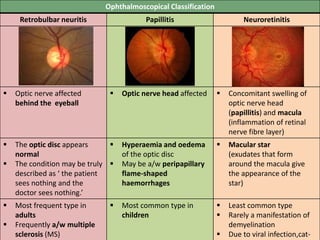
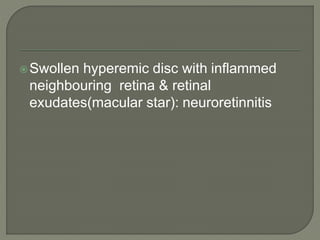
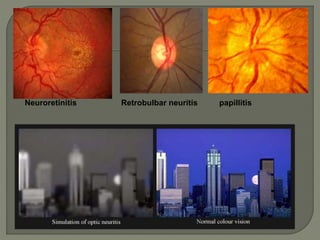
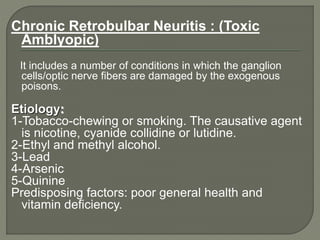
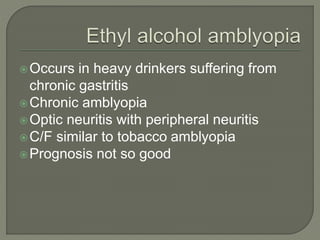
- It is classified ophthalmoscopically into retrobulbar neuritis, papillitis, and neuroretinitis depending on the location of nerve involvement.
- Common causes include multiple sclerosis, infections, and autoimmune disorders.
- Clinical features include acute unilateral vision loss, eye pain on movement, and color vision changes.
- MRI of the brain and orbits with contrast is useful to evaluate for other