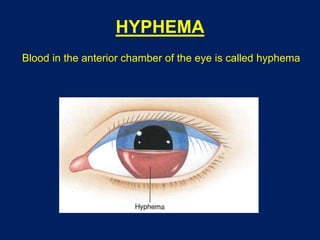
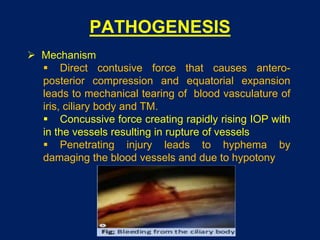
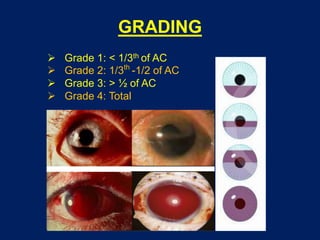
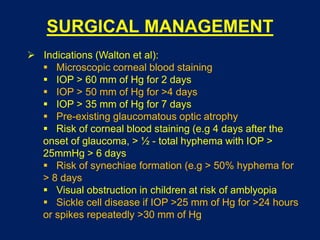
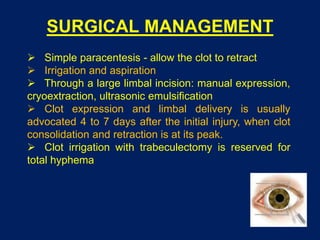
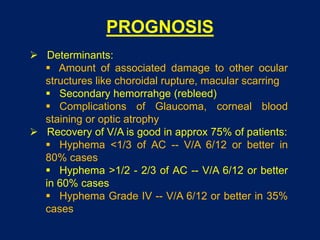
This document discusses hyphema, which is blood in the anterior chamber of the eye. It defines hyphema and lists its potential causes such as trauma, medical conditions, and surgeries/medications. The document outlines methods for grading hyphema based on the amount of blood in the anterior chamber. It also discusses the clinical features, workup, potential complications like increased eye pressure, and treatment approaches like medical management with anti-inflammatory drugs and surgery if needed to prevent complications. The prognosis depends on factors like the severity of hyphema and any associated eye damage.