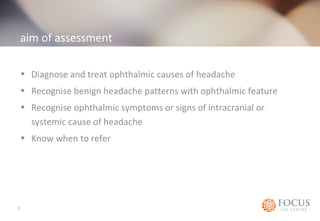
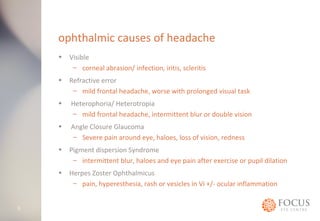
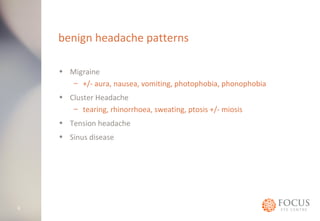
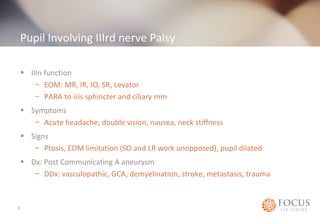
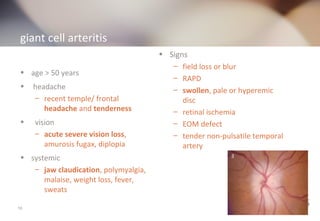
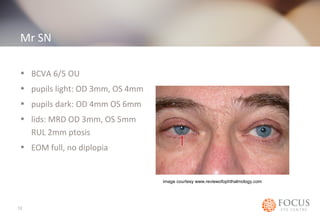
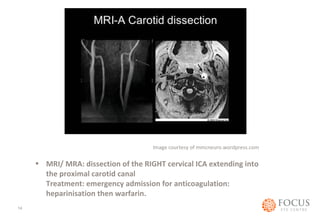
The document discusses the assessment and management of headaches in ophthalmology, detailing symptoms, diagnostic processes, and identifying potential ophthalmic and intracranial causes. It highlights conditions such as migraines, cluster headaches, and the significance of recognizing alarming signs indicative of serious conditions like tumors or vascular issues. It concludes with a case study illustrating a diagnosis of Horner's syndrome due to internal carotid artery dissection requiring immediate anticoagulation treatment.