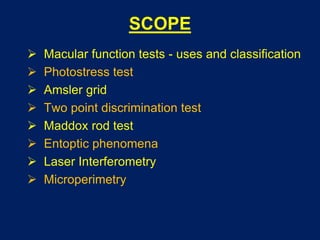
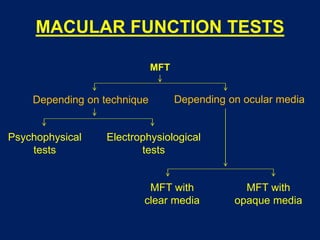
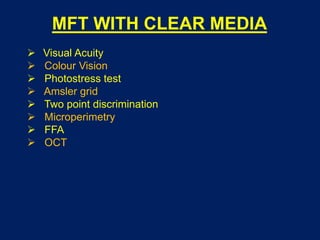
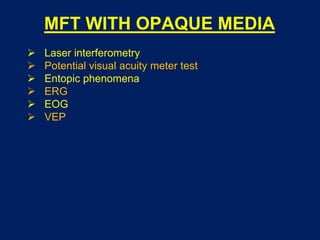
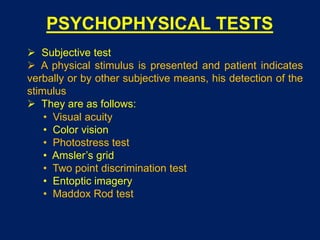
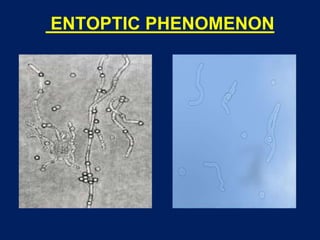
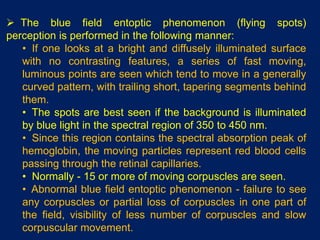
This document discusses various tests used to evaluate macular function, including psychophysical and electrophysiological tests. Psychophysical tests include visual acuity tests, Amsler grid, photostress testing, and two-point discrimination. Electrophysiological tests include ERG, EOG, and VEP. Special tests are used to evaluate macular function in eyes with opaque media, such as laser interferometry, potential visual acuity meter, and entoptic phenomena observation. Microperimetry allows precise correlation of retinal sensitivity with fundus details. No single test evaluates all aspects of macular function, so multiple tests are often used.