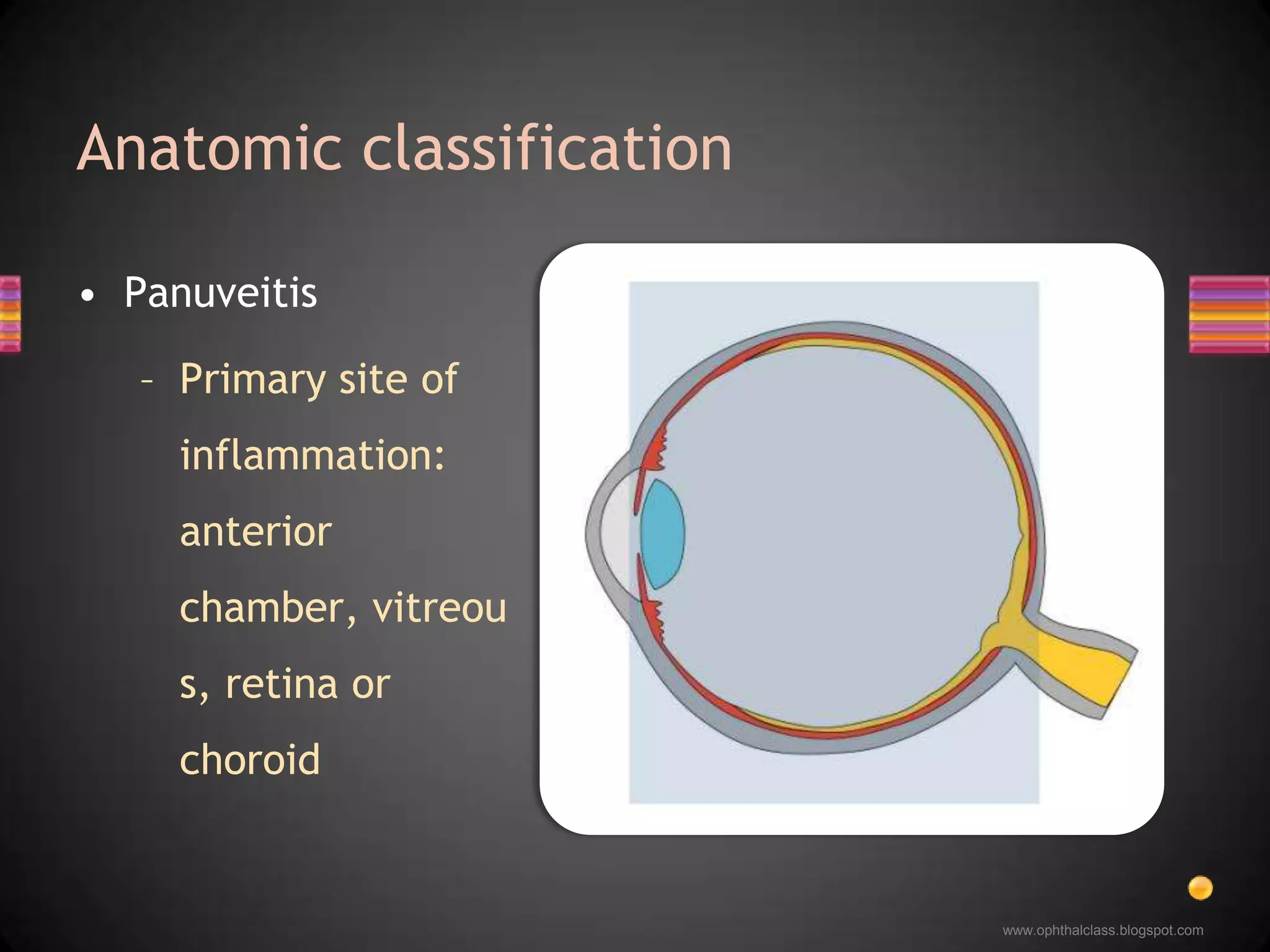
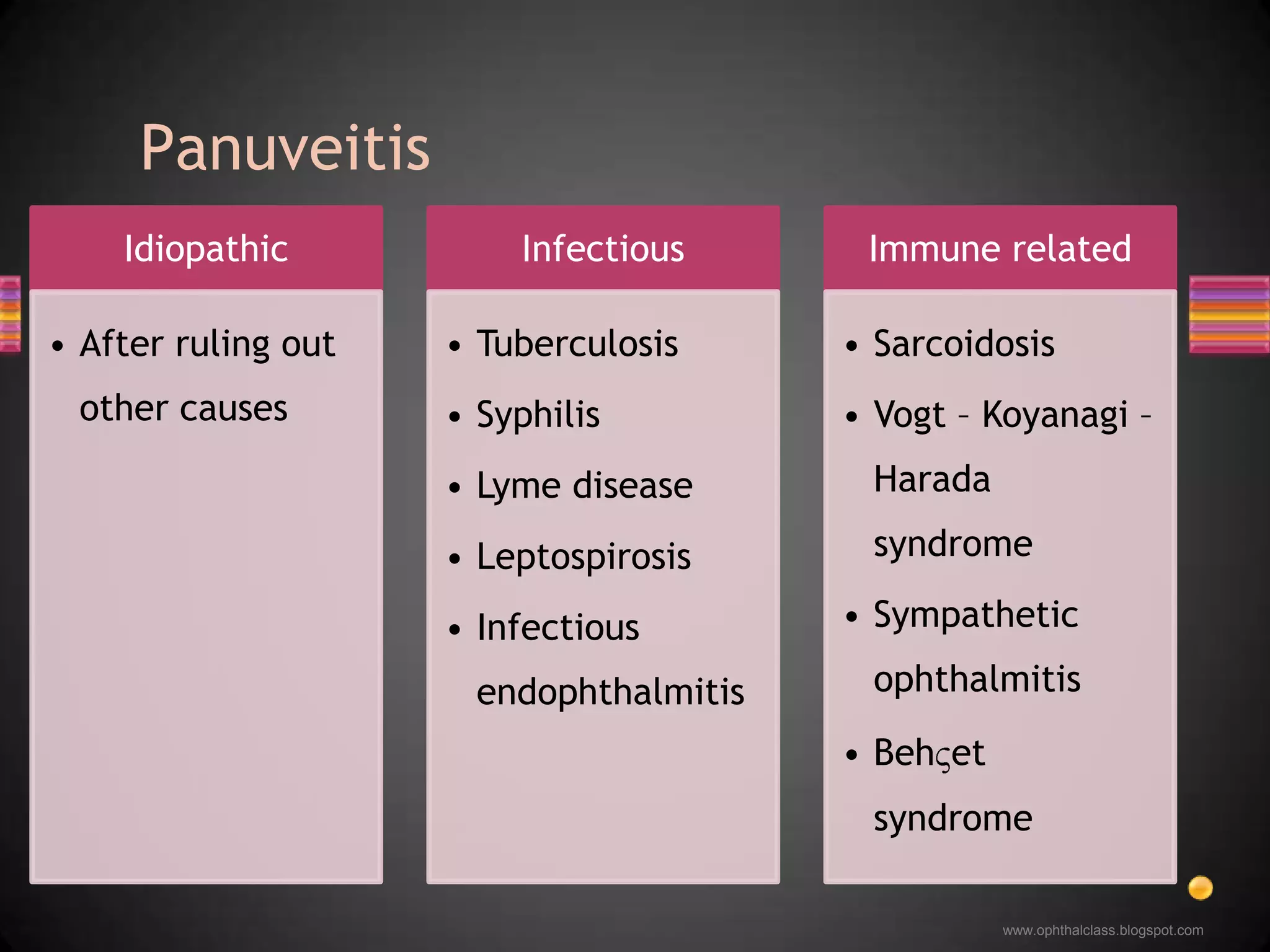
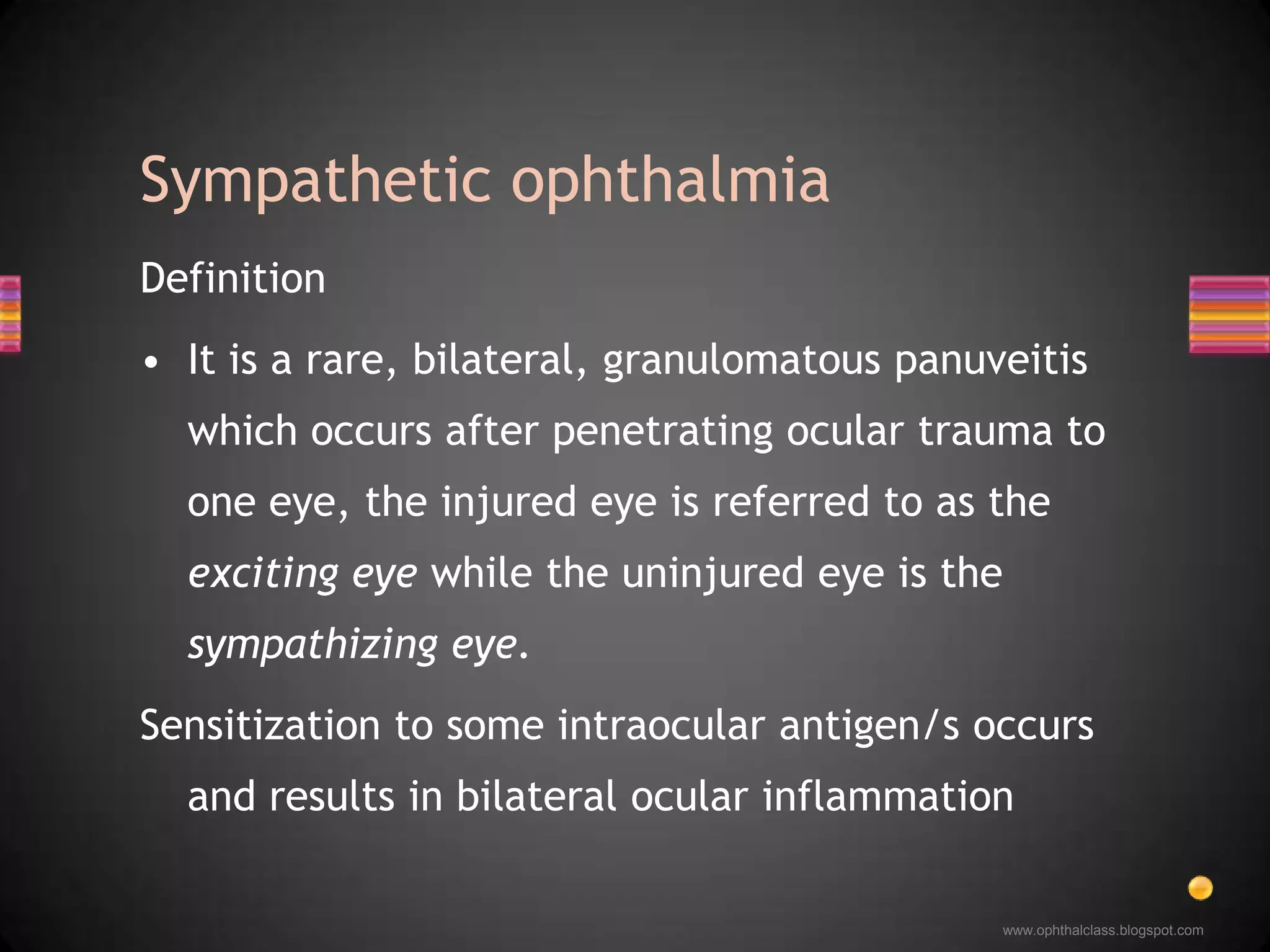
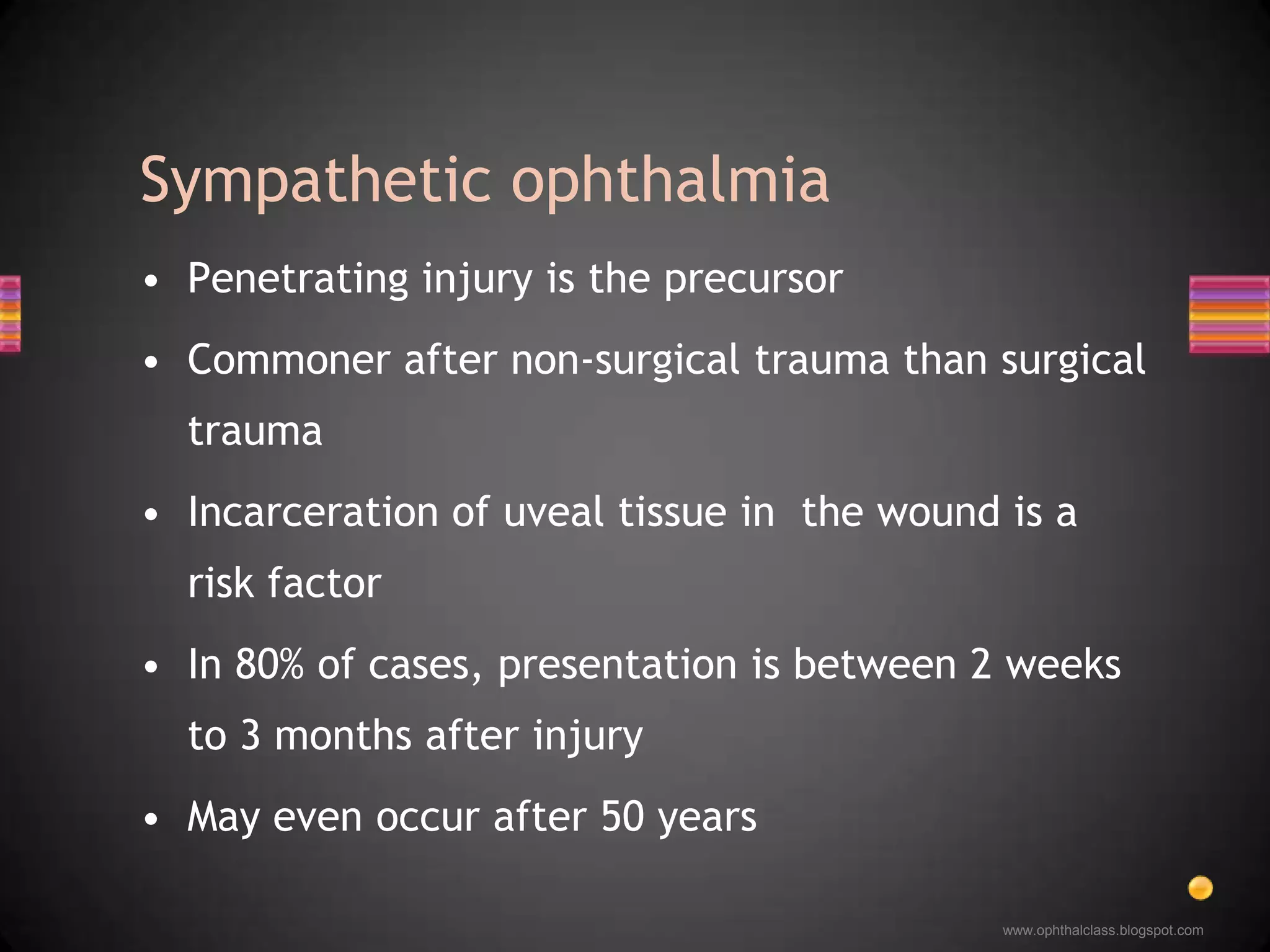
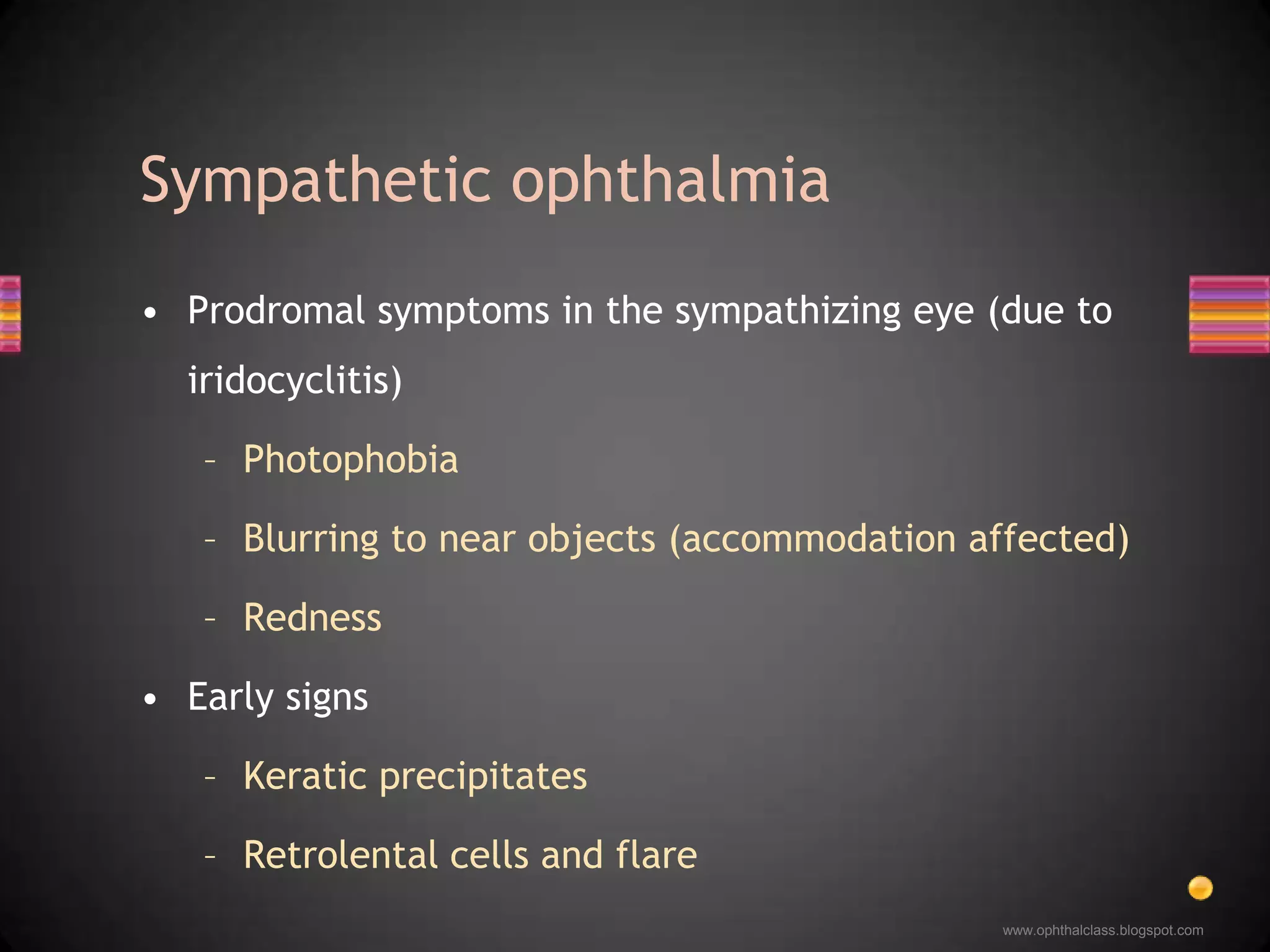
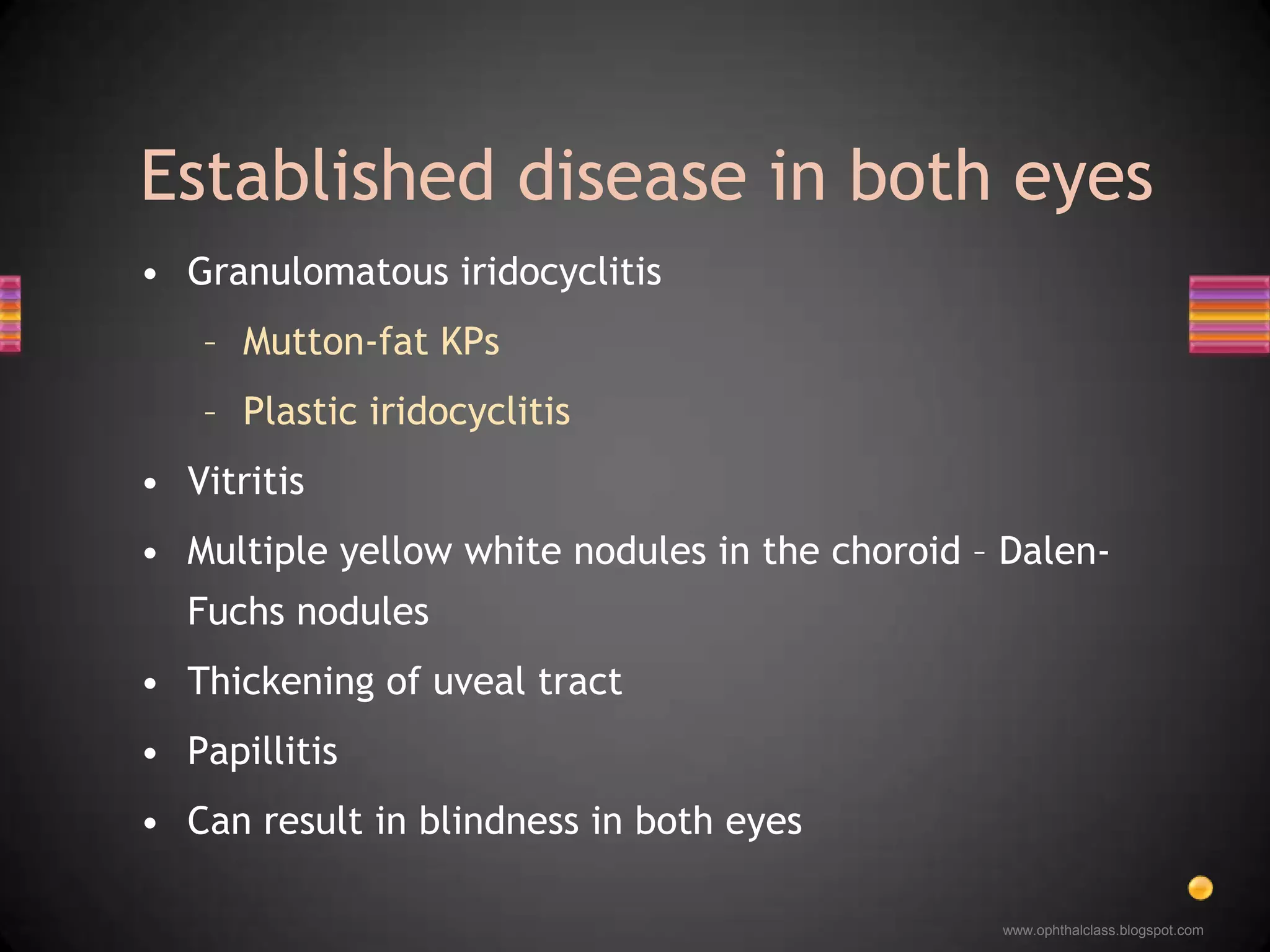
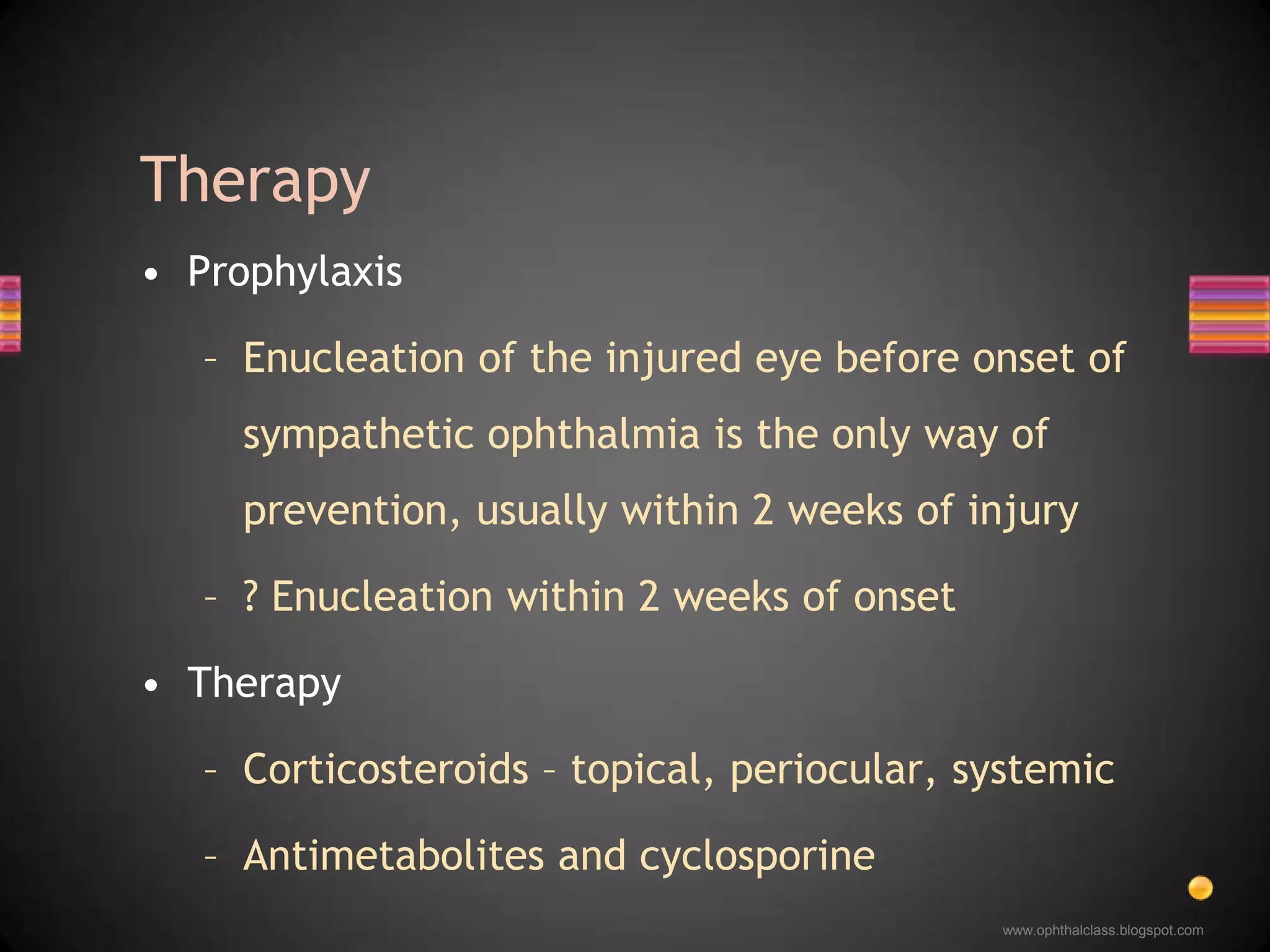
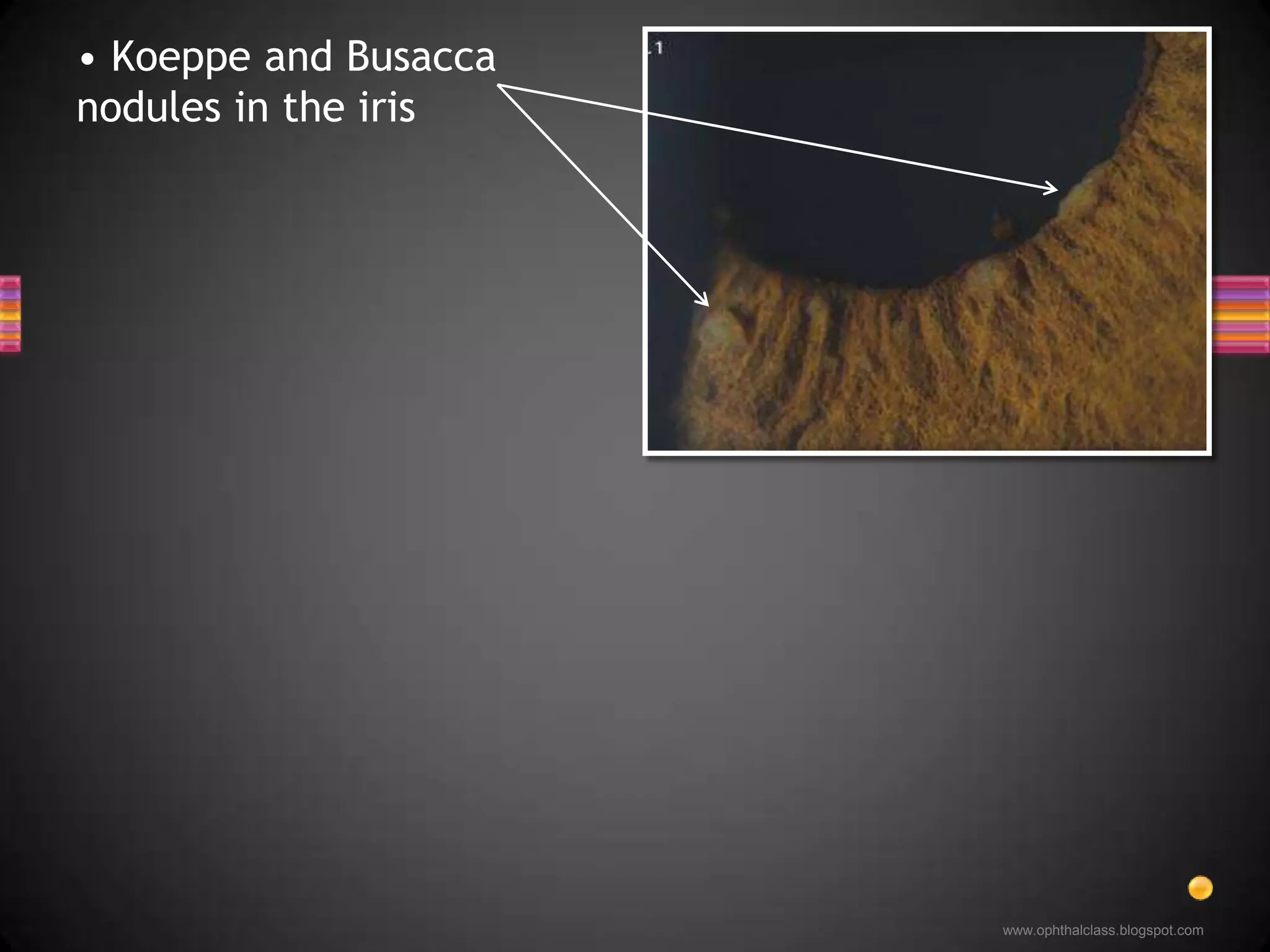
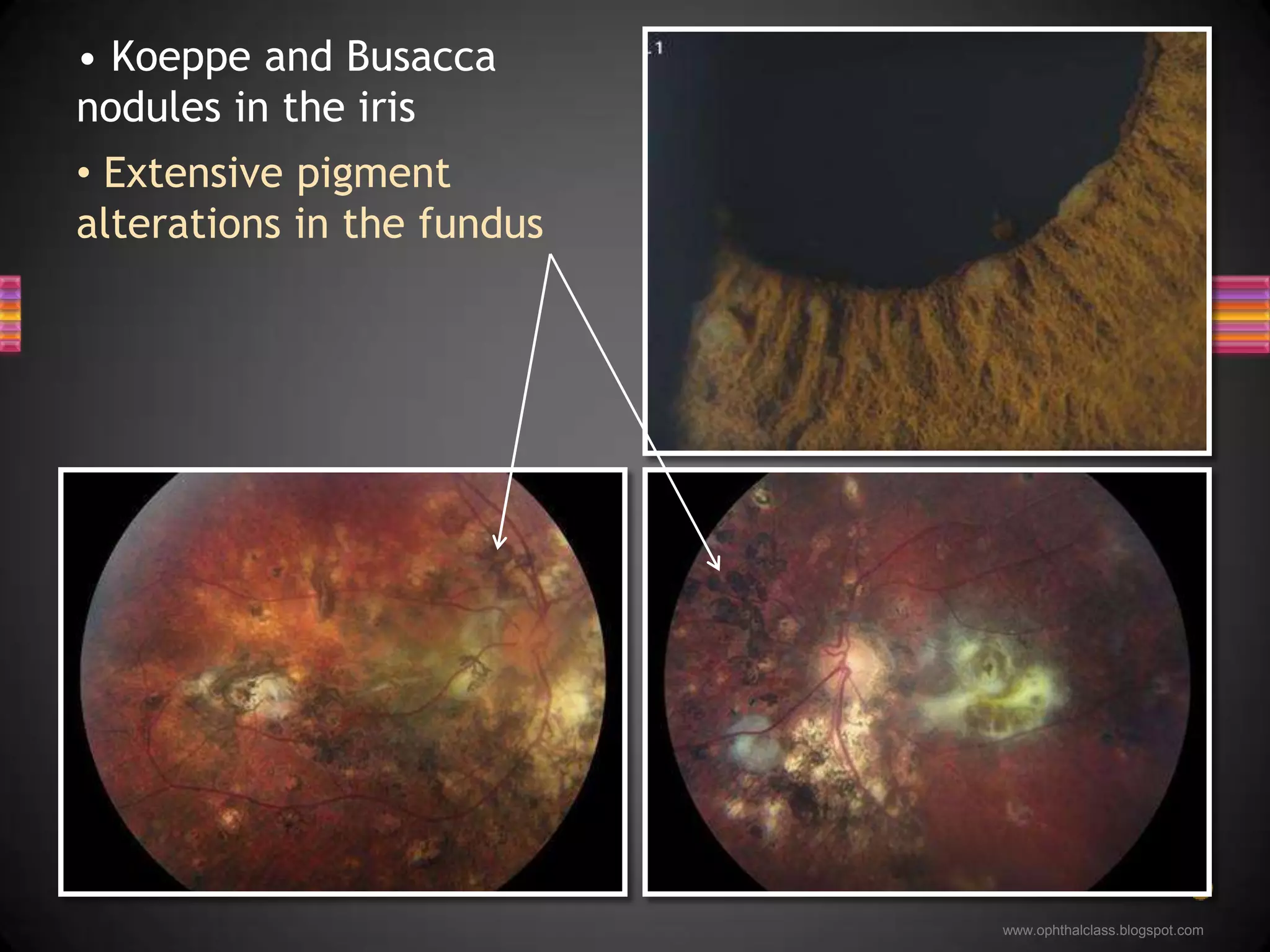
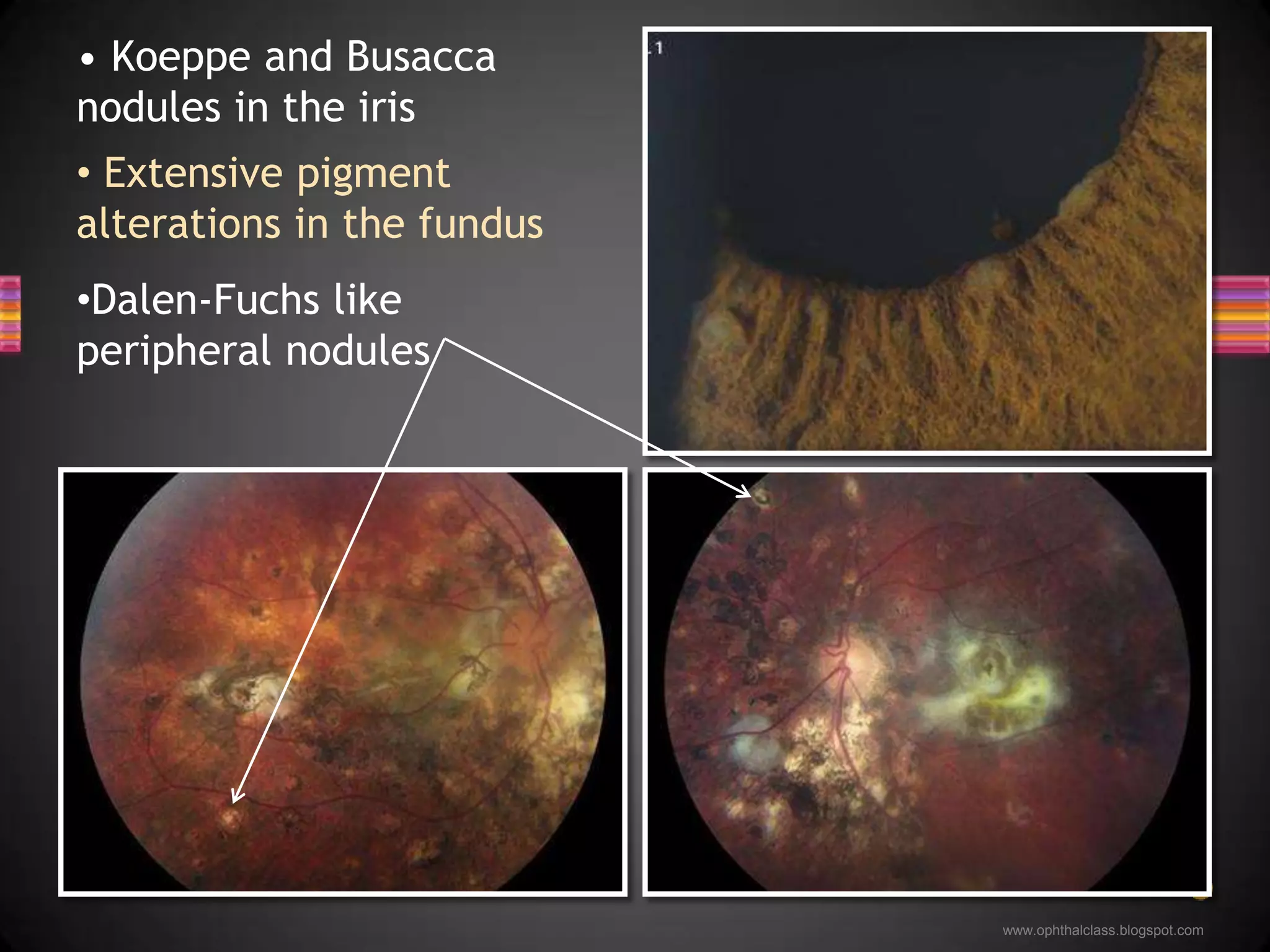
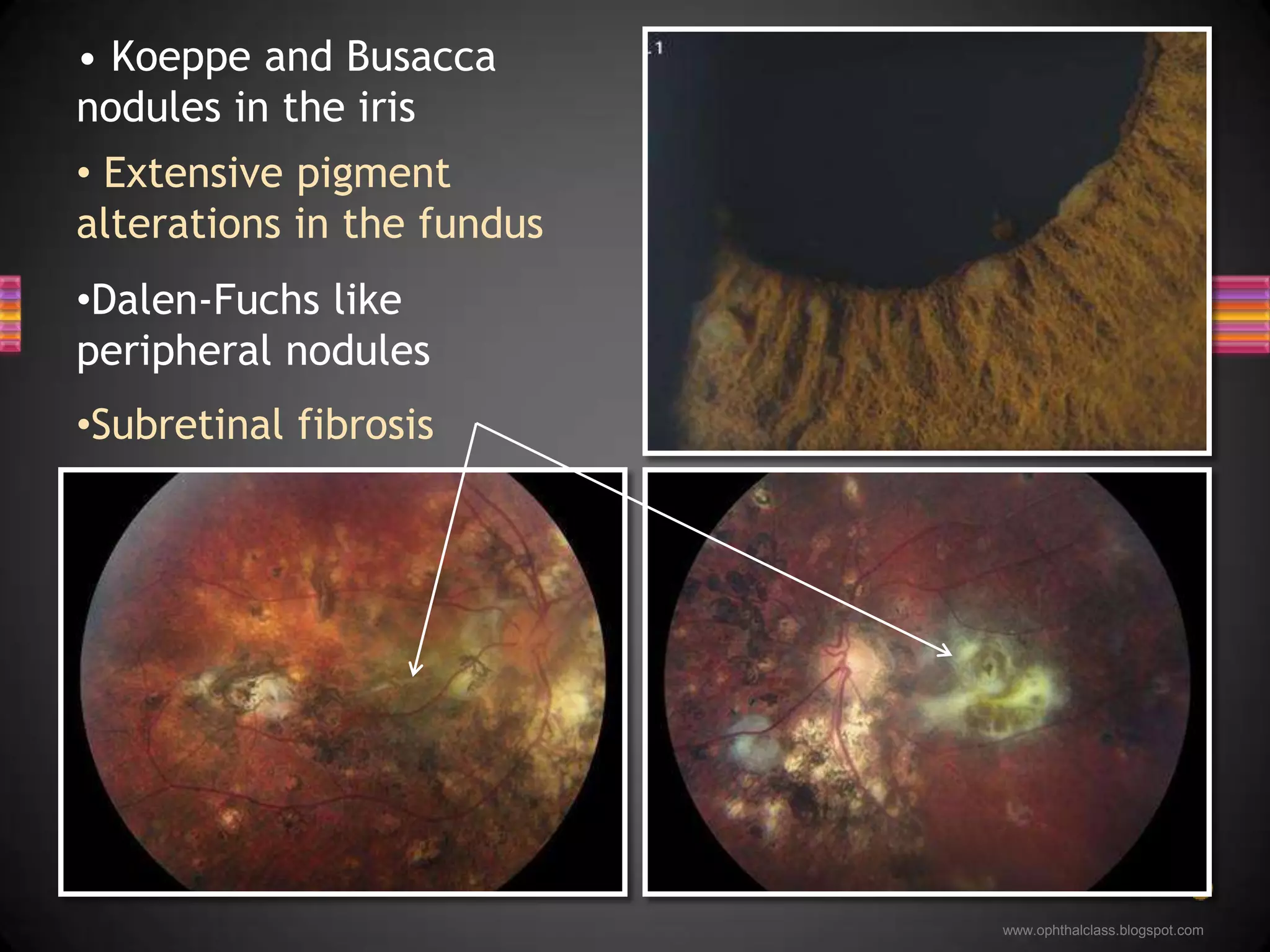
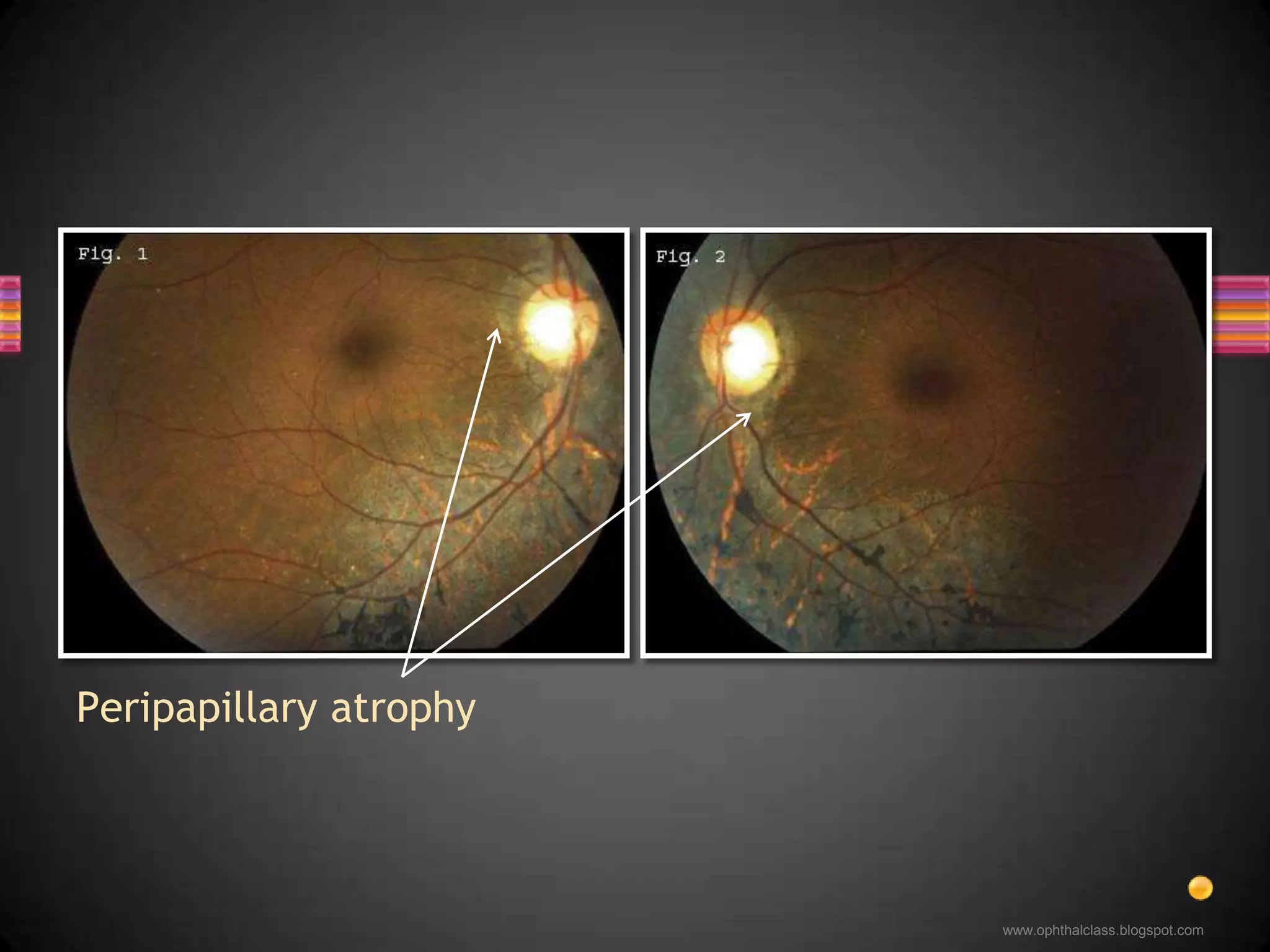
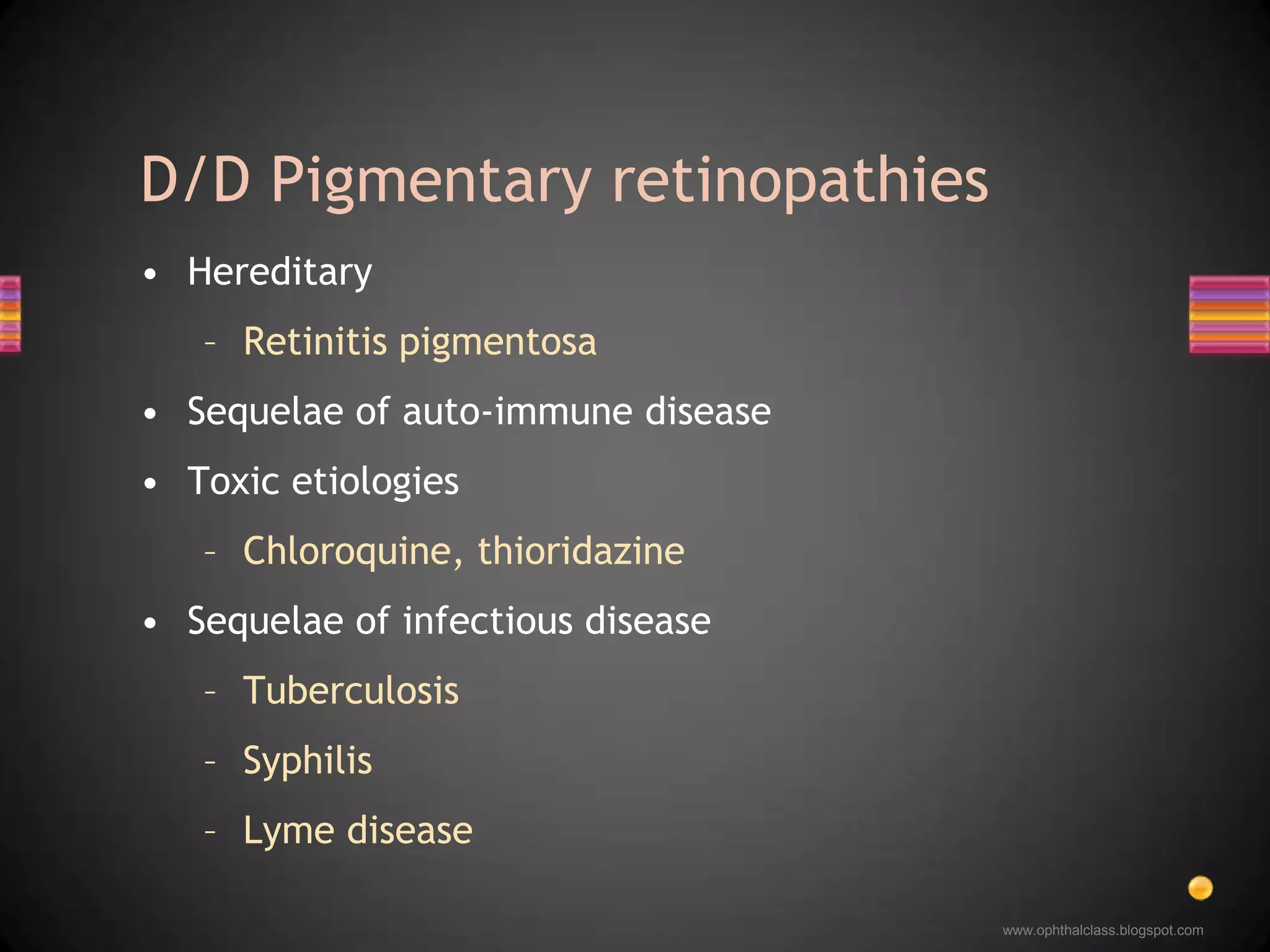
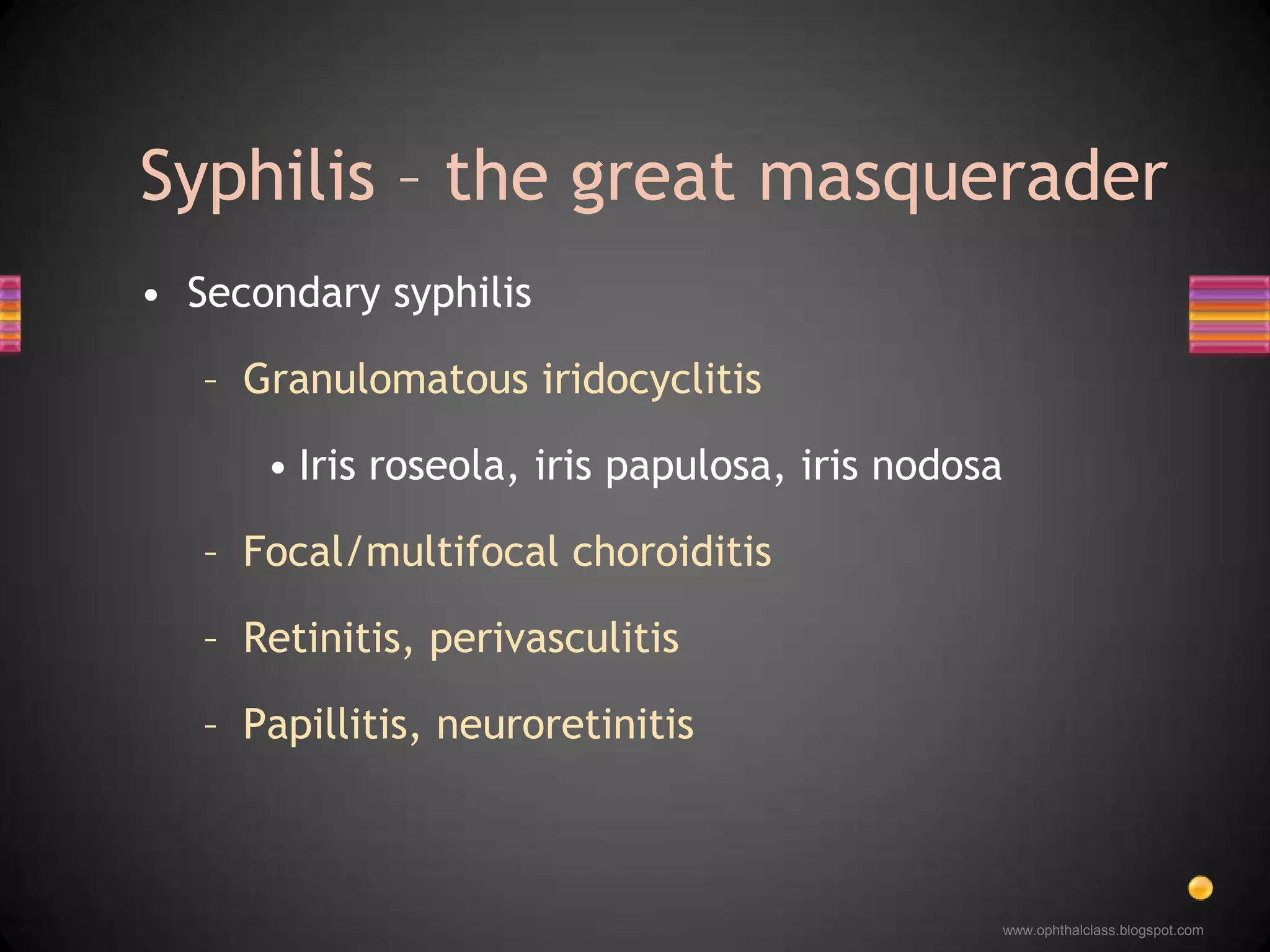
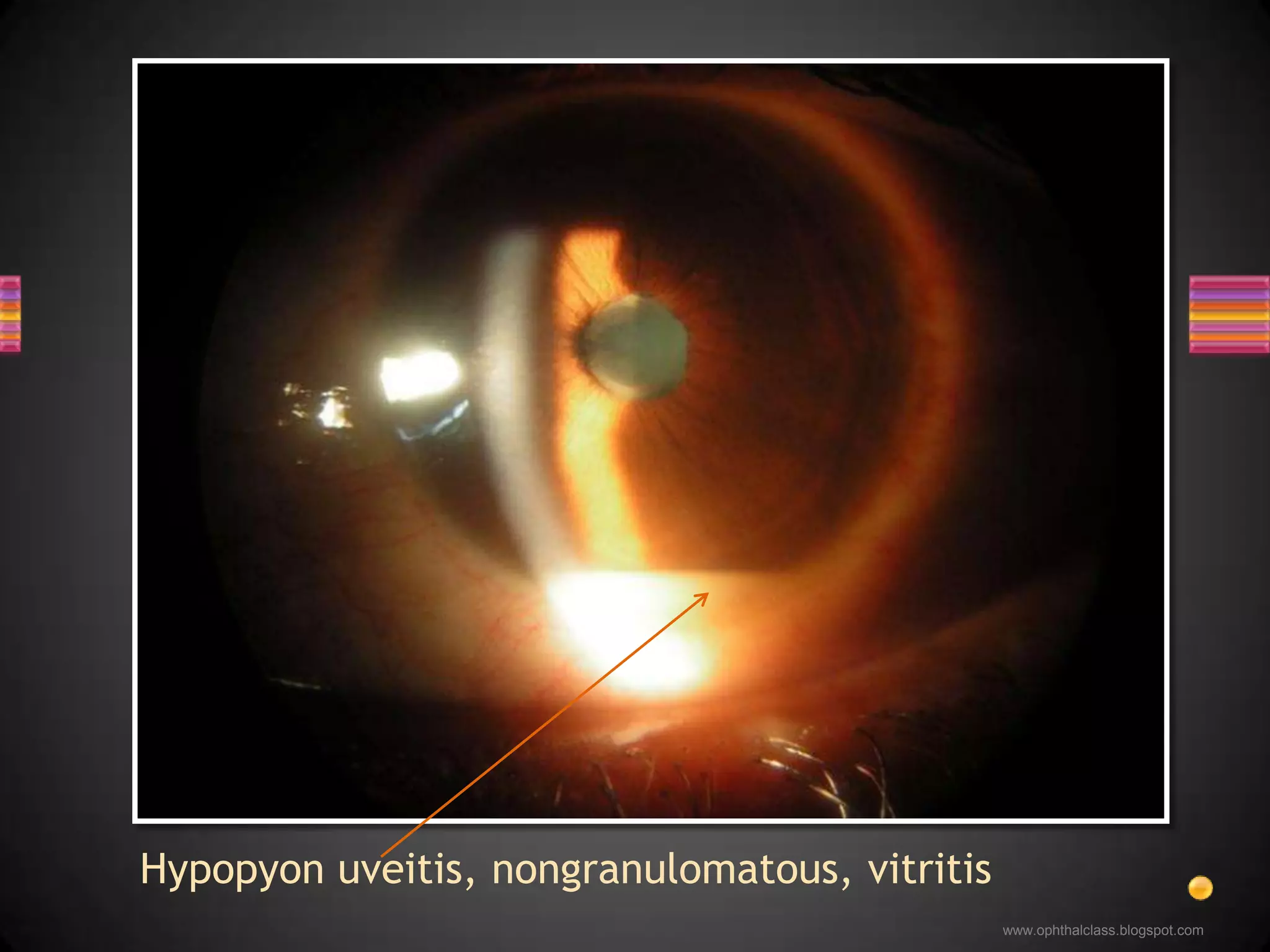
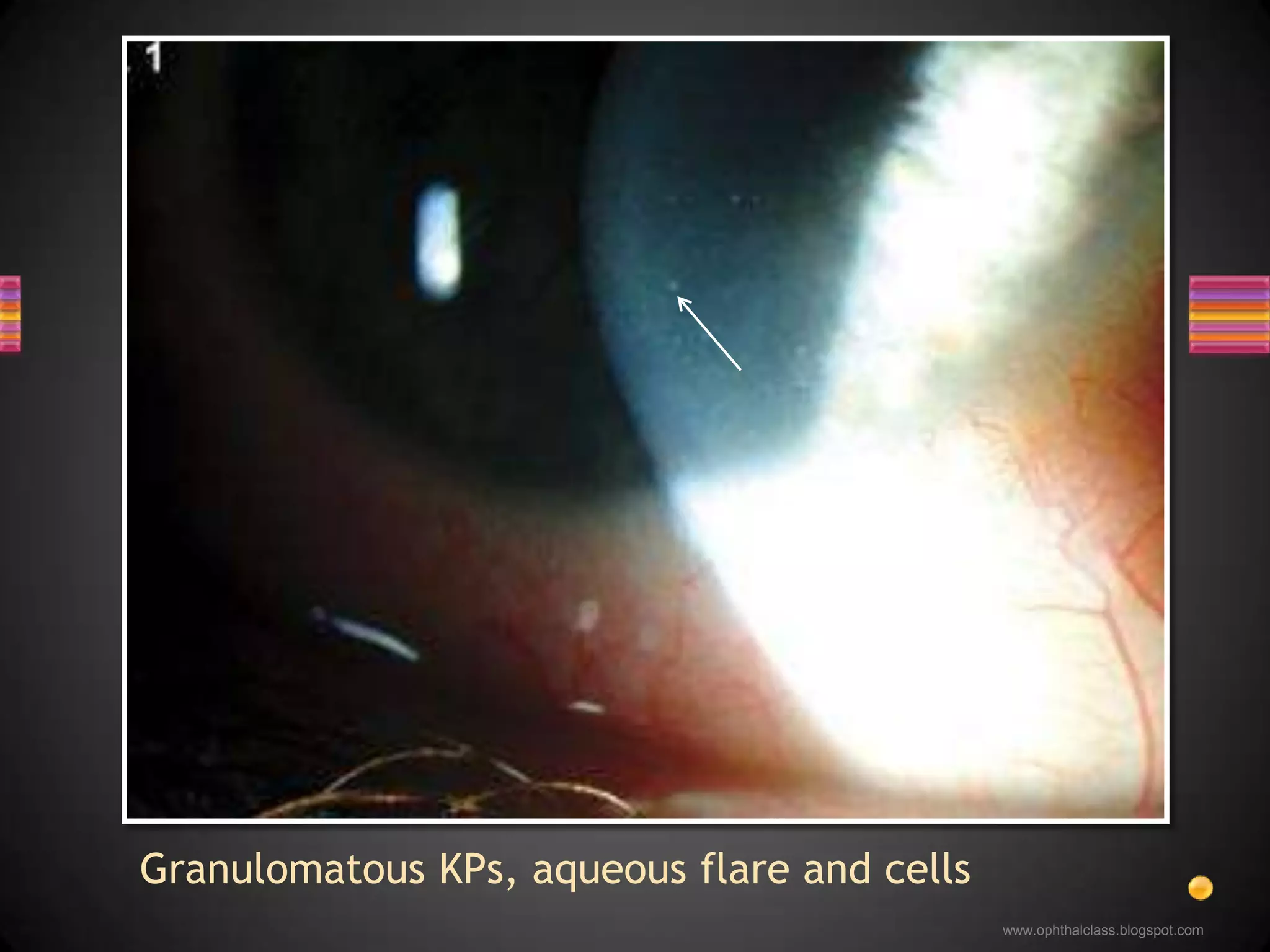
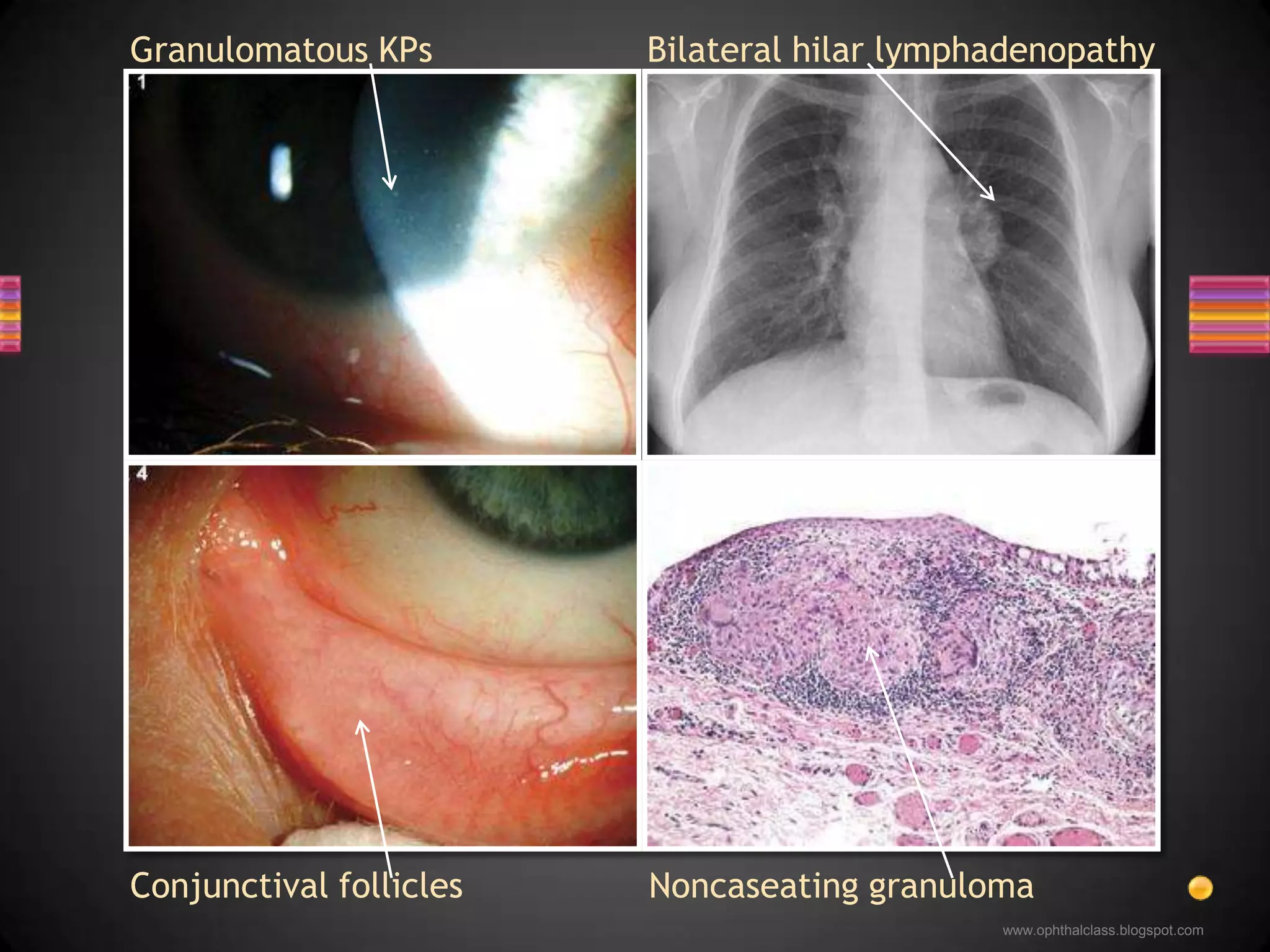
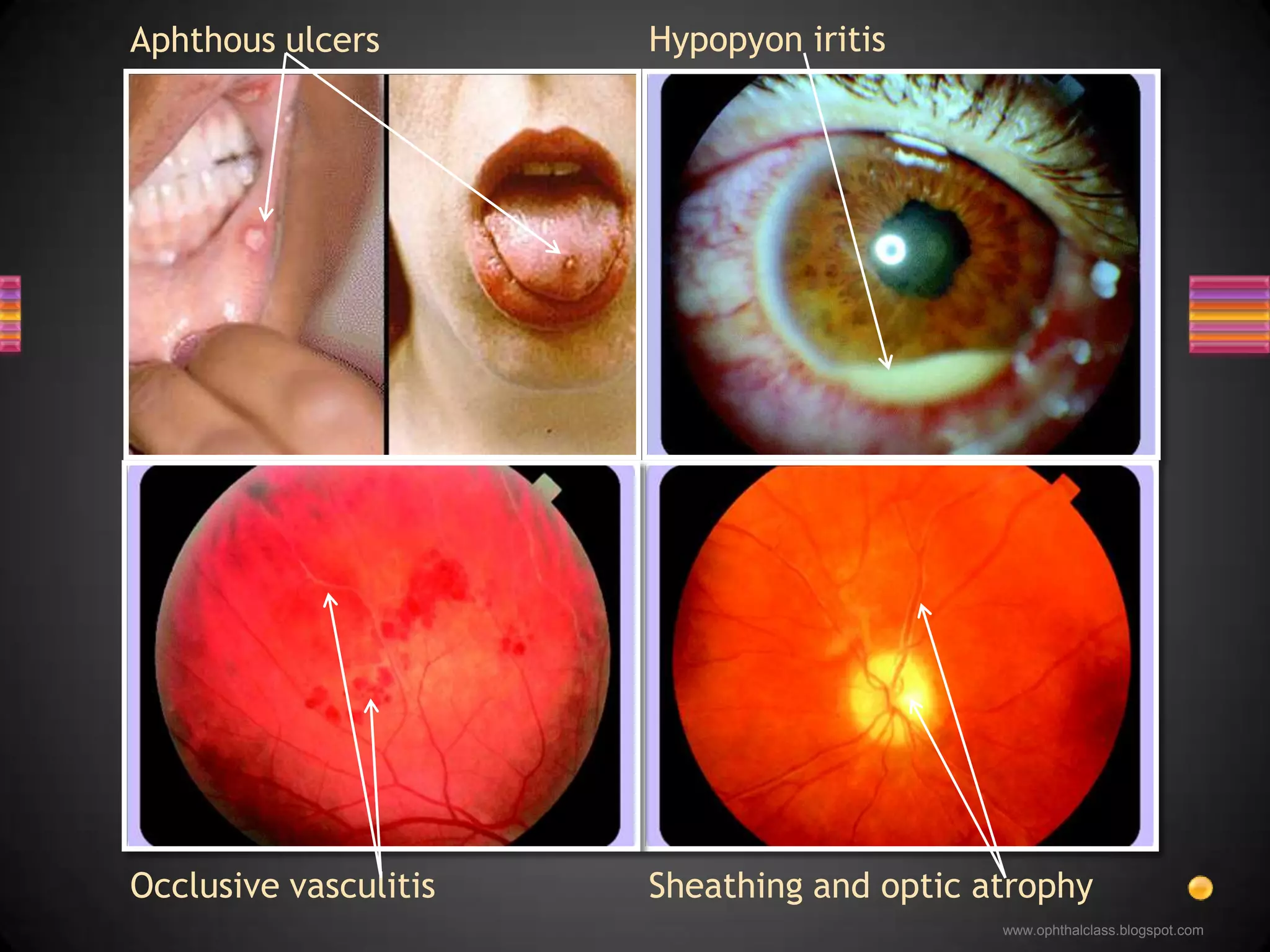
The document provides an overview of various forms of uveitis, including panuveitis, and outlines their classifications, causes, and management strategies. It elaborates on sympathetic ophthalmia as a severe form of panuveitis that can arise after ocular trauma, alongside details of other conditions like Vogt-Koyanagi-Harada disease and sarcoidosis. Treatment options primarily include corticosteroids and immunosuppressives, with specific considerations given to the etiology, such as infections or autoimmune diseases.