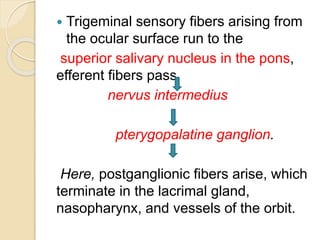
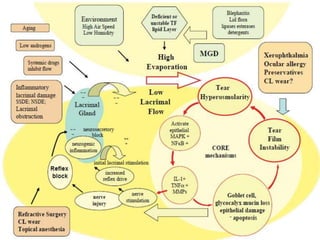
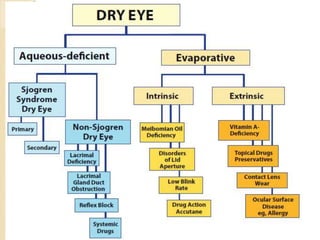
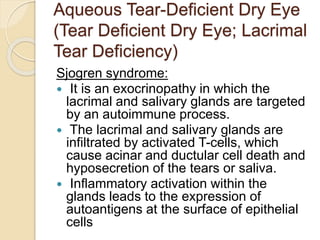
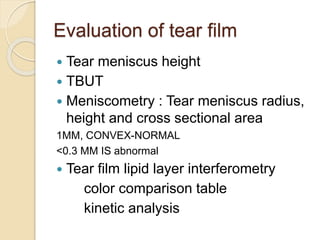
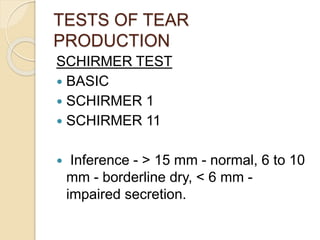
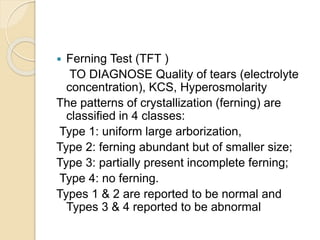
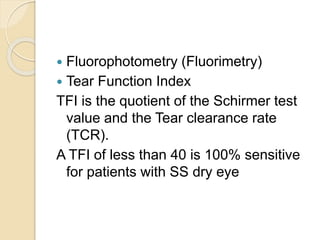
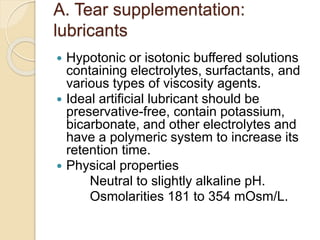
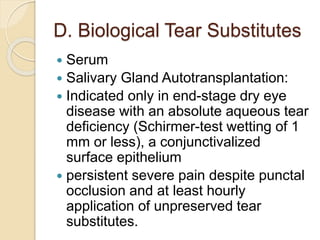
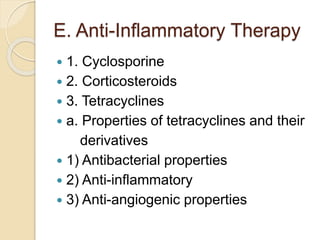
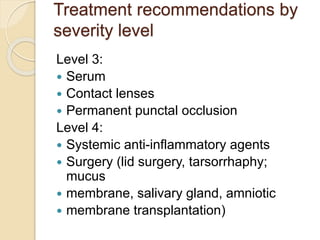
Dry eye is a disease of the tear film and ocular surface caused by reduced tear production or increased tear evaporation. It results in eye discomfort, visual disturbance, and potential ocular surface damage. Dry eye can be caused by problems with the lacrimal functional unit such as aging, autoimmune disease like Sjogren's syndrome, or environmental factors. Diagnosis involves evaluating tear production via tests like Schirmer's test and tear breakup time, and assessing ocular surface staining. Treatment depends on dry eye severity and may include artificial tears, anti-inflammatories, punctal plugs, and management of underlying conditions. The goal is to supplement tears, reduce evaporation, stimulate natural tear production, and minimize