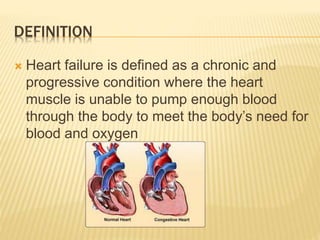
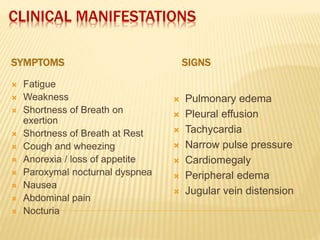
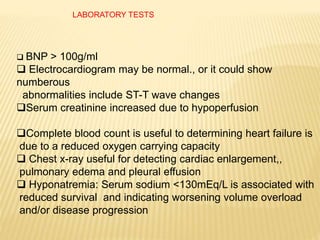
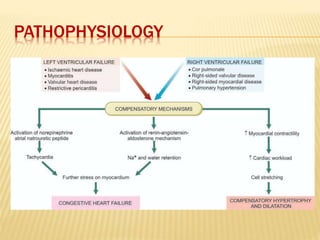
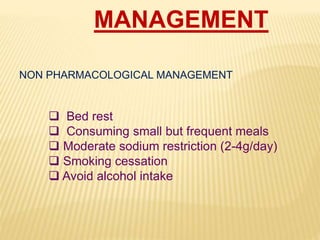
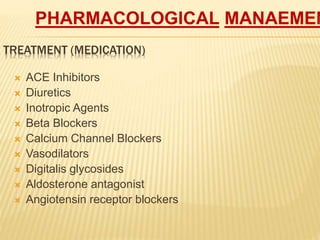
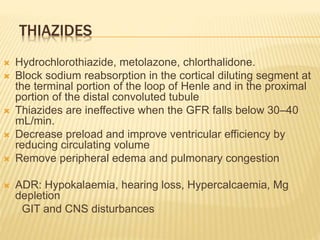
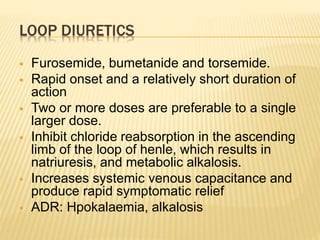
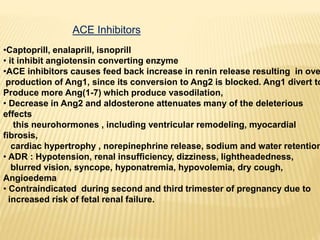
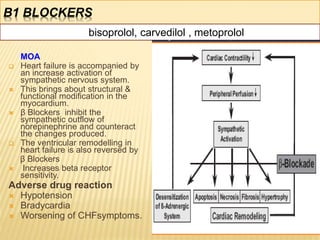
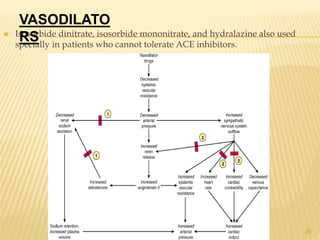
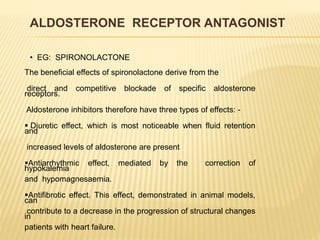
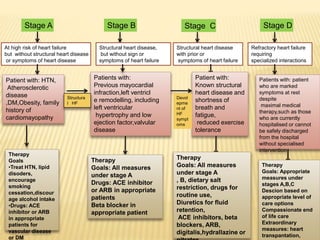
Congestive cardiac failure is defined as a chronic condition where the heart is unable to pump enough blood to meet the body's needs. It can be classified as systolic, diastolic, acute or chronic. Common causes include arrhythmias, myocardial infarction, hypertension, and obesity. Symptoms include fatigue, shortness of breath, and edema while signs include tachycardia and edema. Diagnosis involves tests such as ECG, echocardiogram, and blood tests. Management consists of medications like ACE inhibitors, diuretics, beta-blockers and lifestyle modifications like diet, exercise and smoking cessation.