This presentation provides an overview of heart failure, including:
1. It defines heart failure as when the heart is unable to pump sufficiently to meet the body's needs, which can result from systolic or diastolic dysfunction.
2. Some key statistics on the incidence and prevalence of heart failure worldwide and in India are presented.
3. Heart failure is classified in different ways such as whether it affects the left or right side of the heart, and whether it involves forward or backward failure.
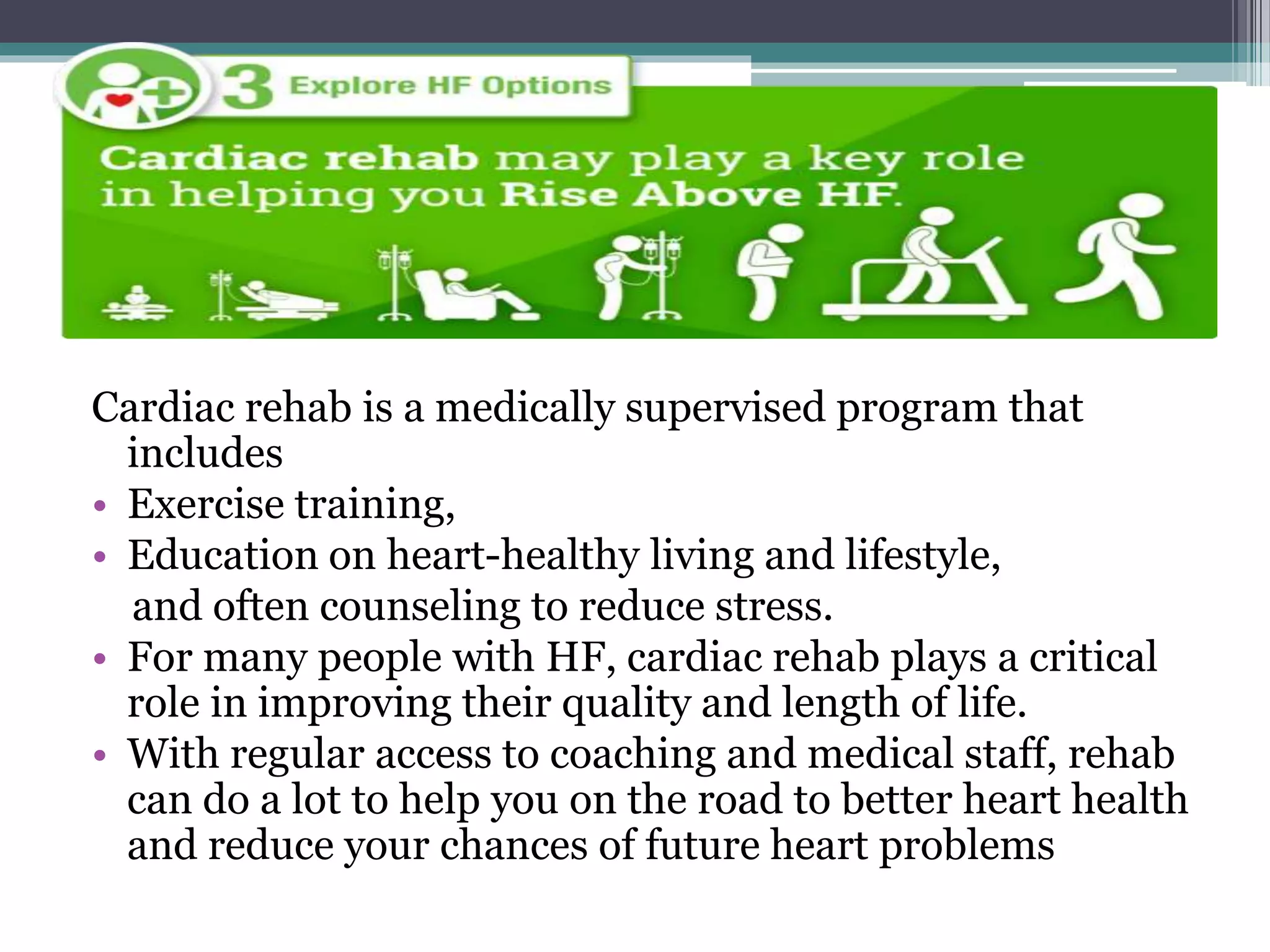
4. The etiology, clinical presentation, diagnostic assessment, medical management including medications, and surgical options for treatment are discussed at a high level.