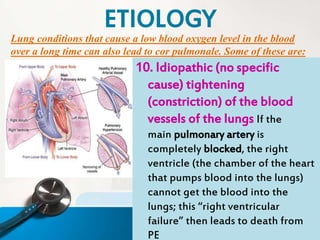
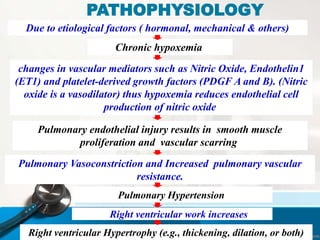
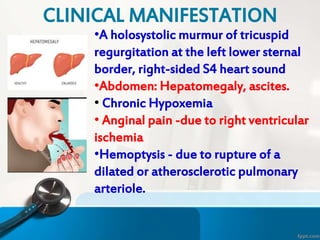
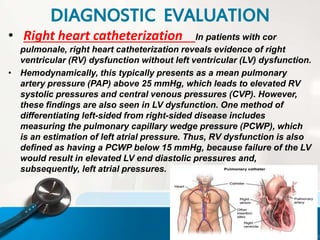
Cor pulmonale is a condition where the right ventricle of the heart enlarges and fails due to high blood pressure in the pulmonary arteries, usually caused by long-term lung diseases that reduce oxygen levels. It most commonly results from chronic obstructive pulmonary disease (COPD). Symptoms include shortness of breath, swelling, and chest pain. Diagnosis involves physical exam, imaging, blood tests, and right heart catheterization. Treatment focuses on improving oxygen levels, reducing pulmonary pressures, and managing the underlying lung condition.