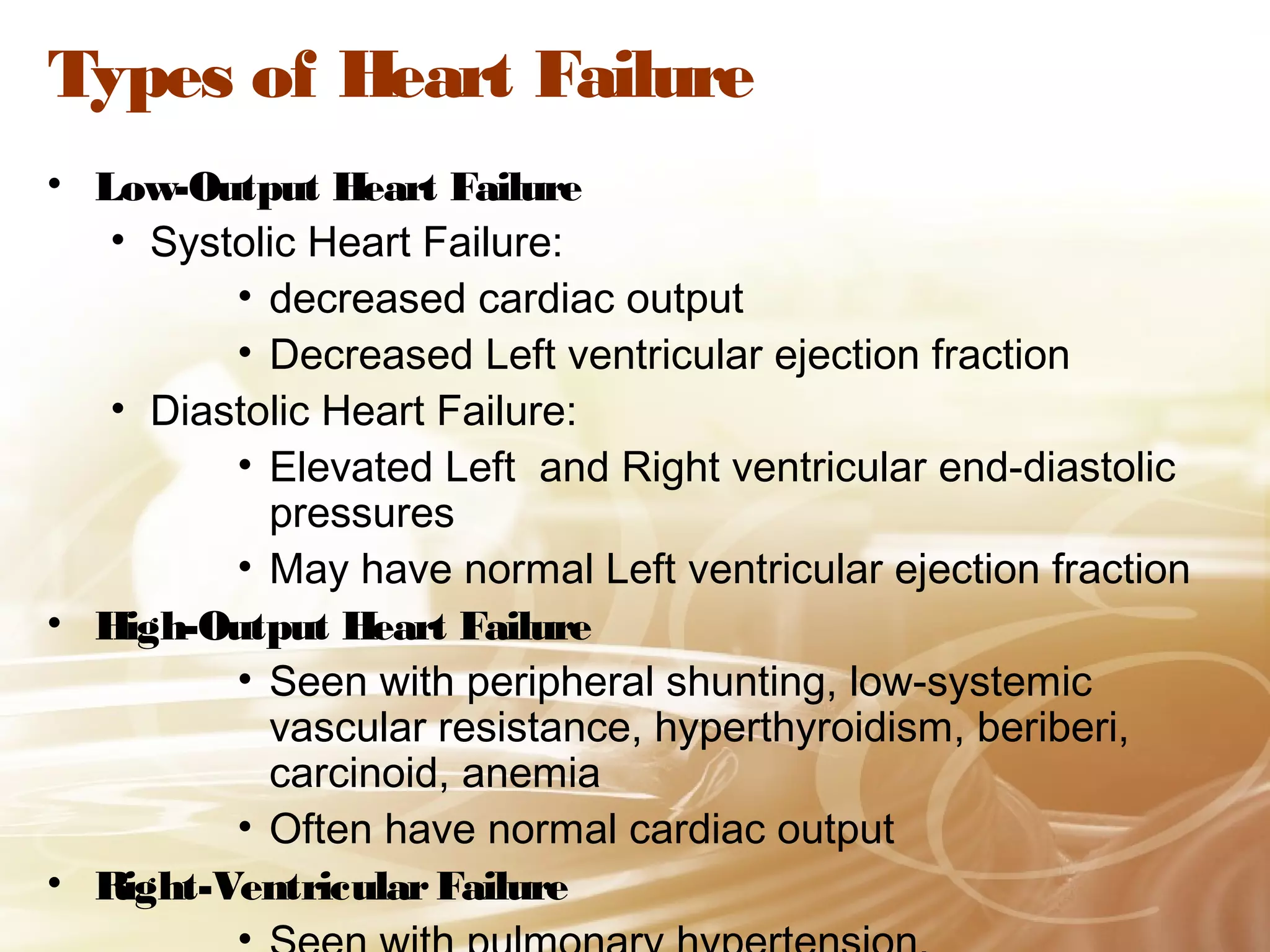
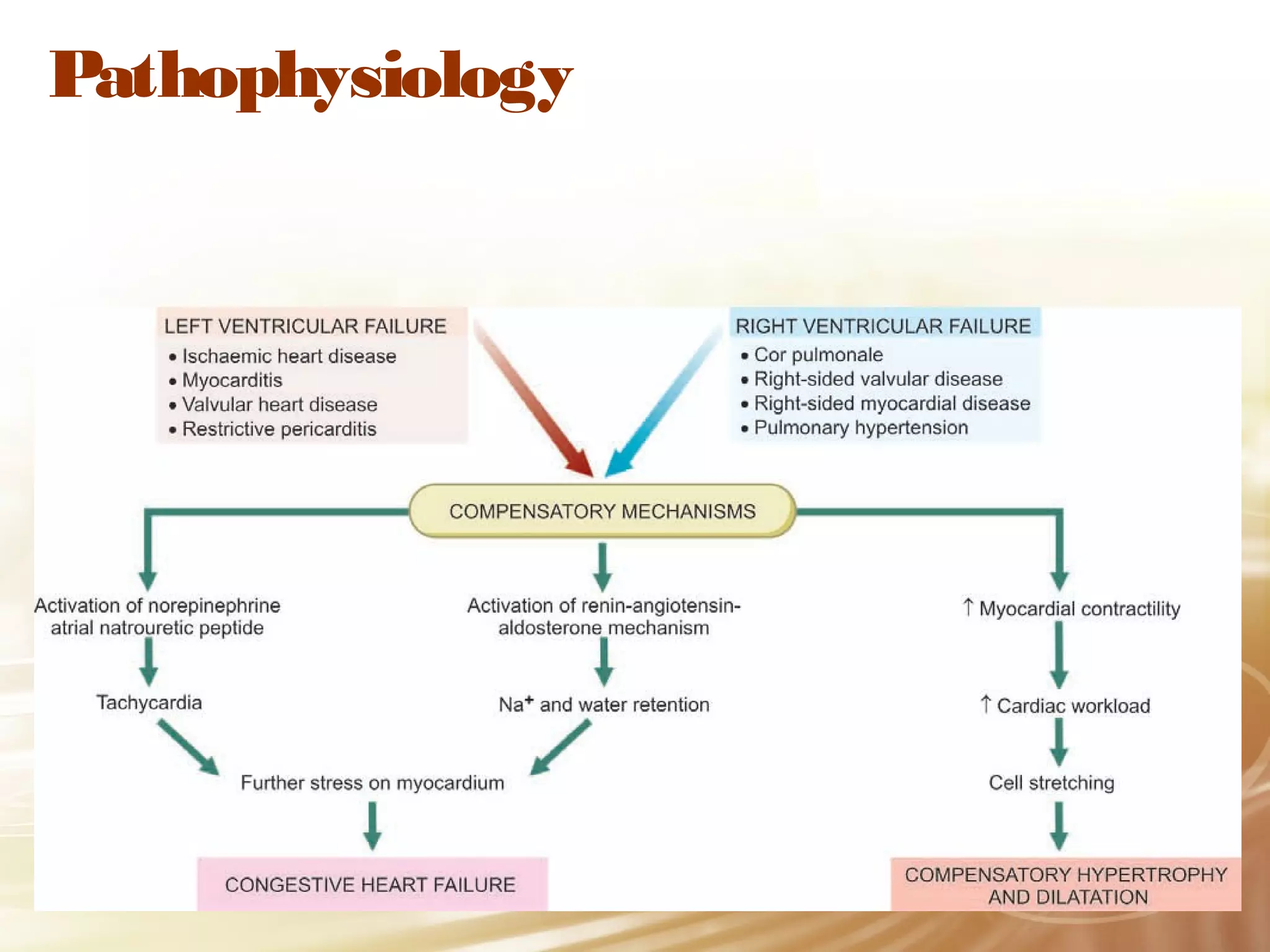
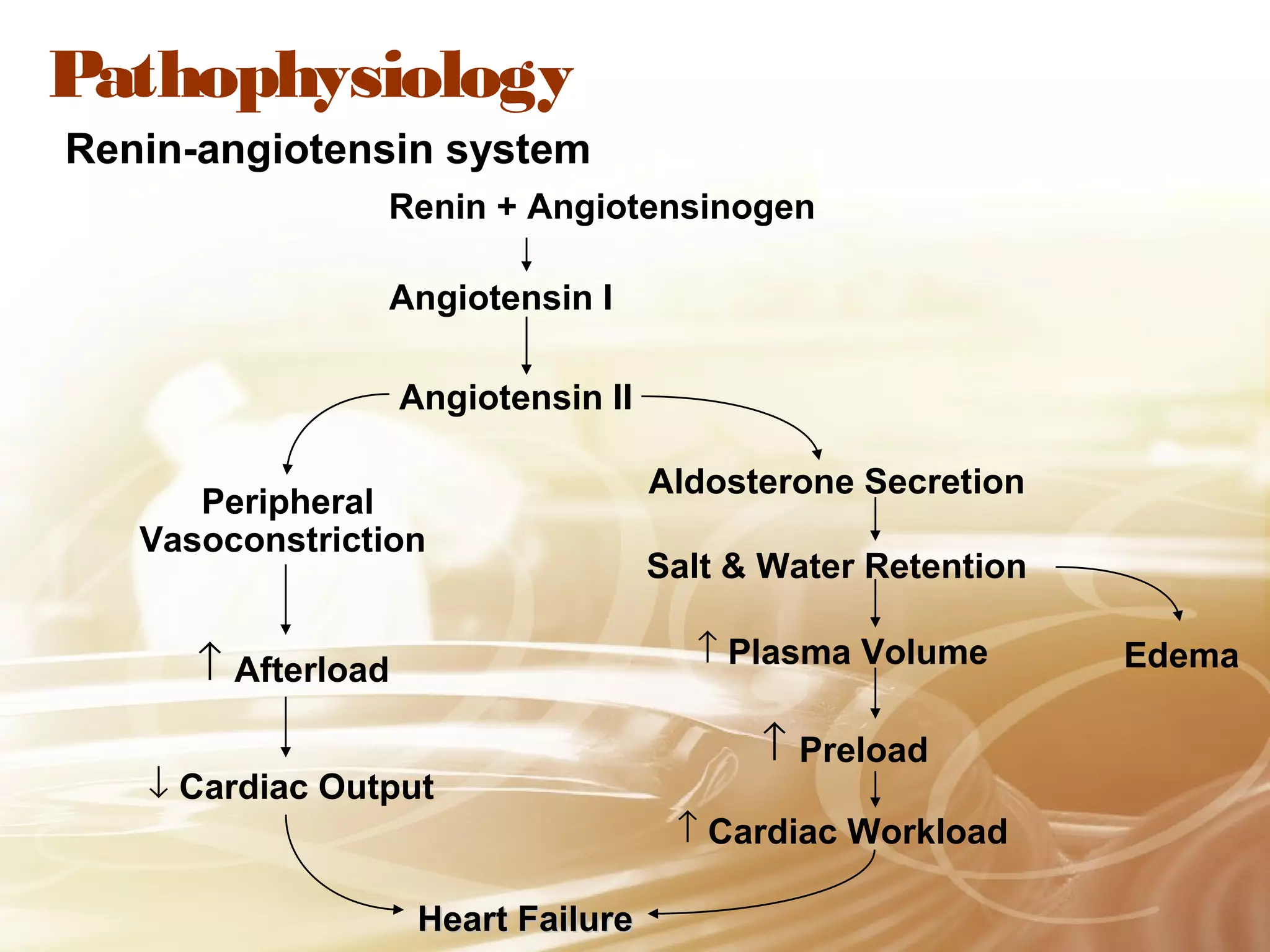
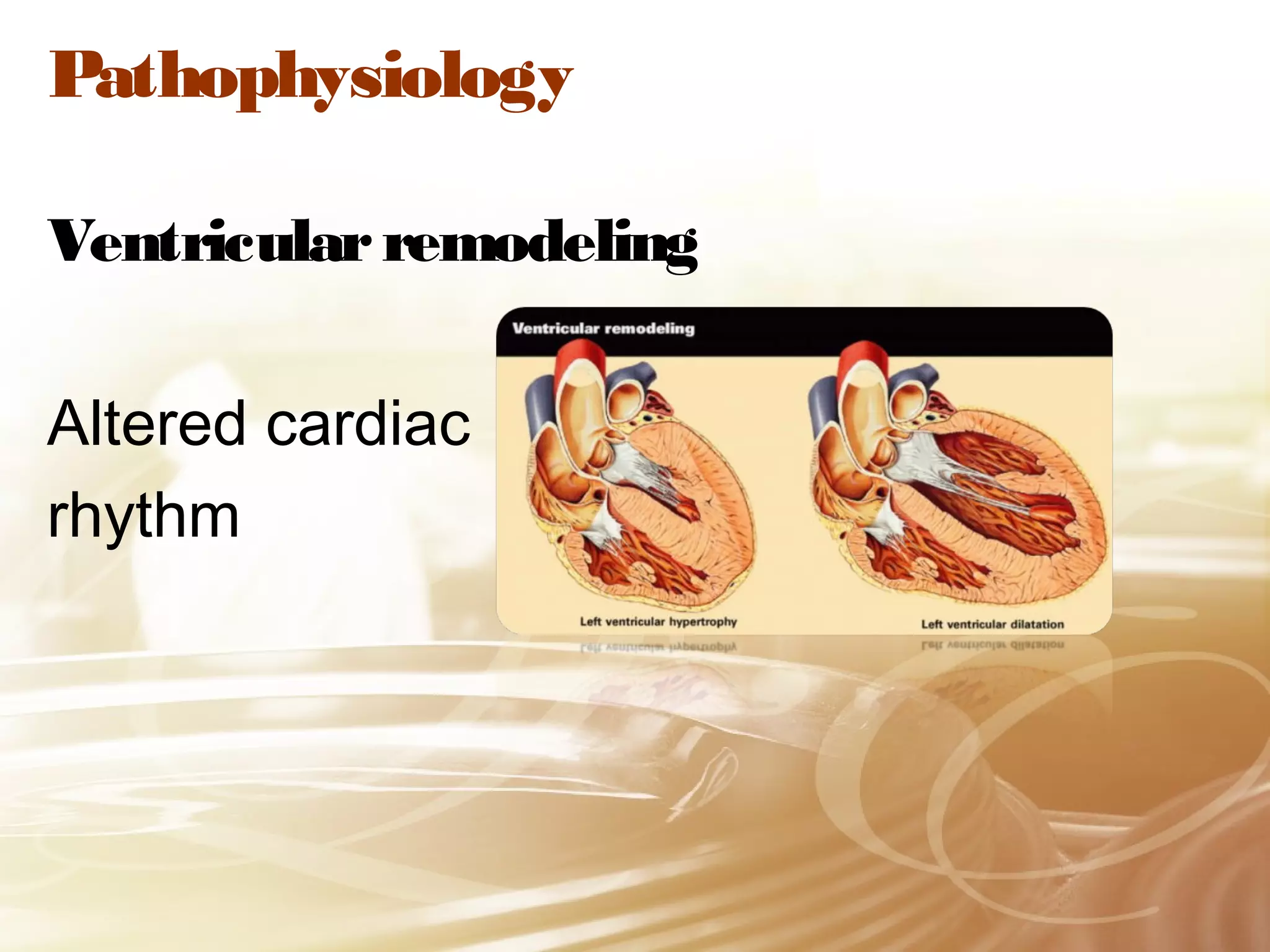
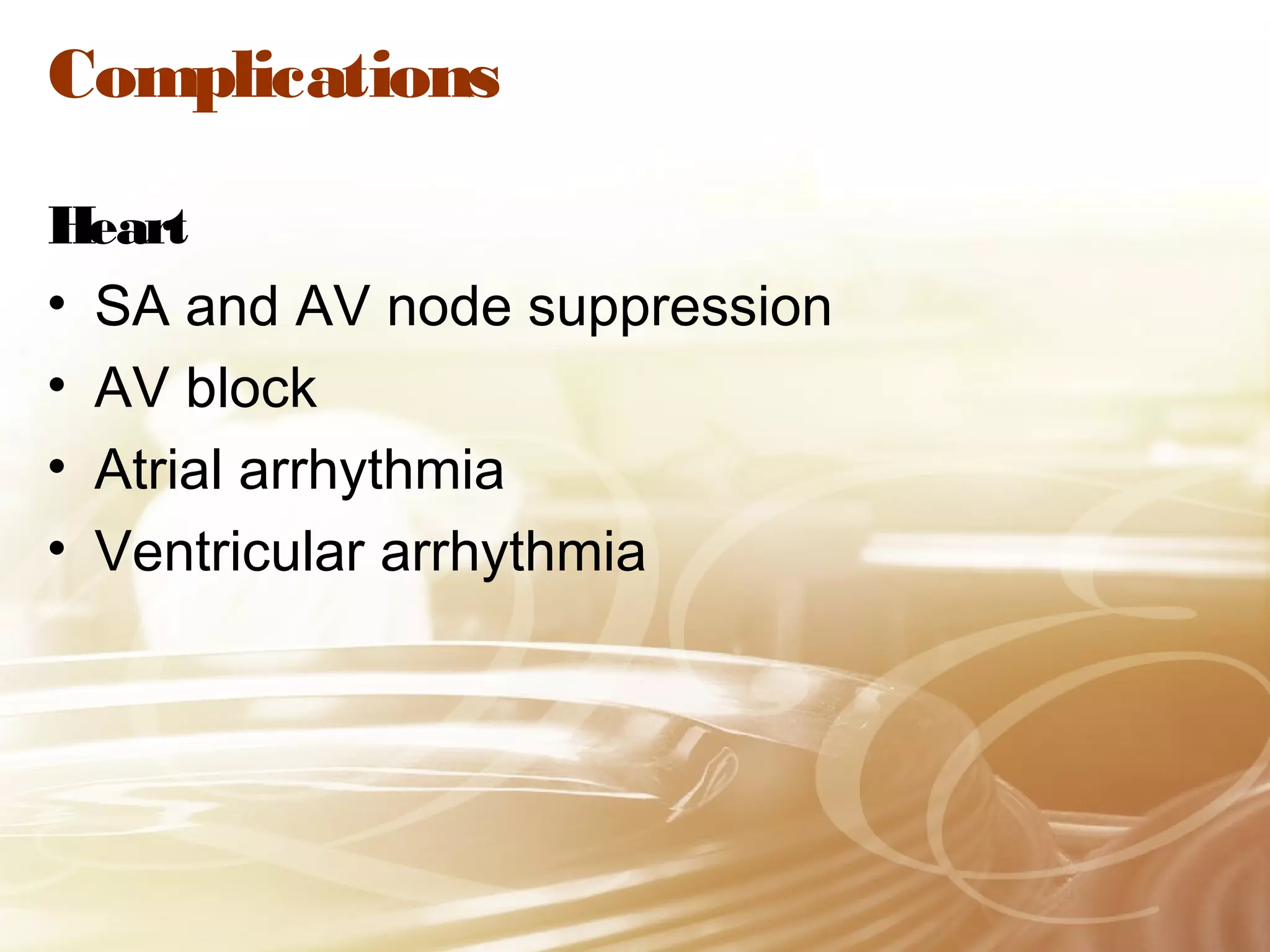
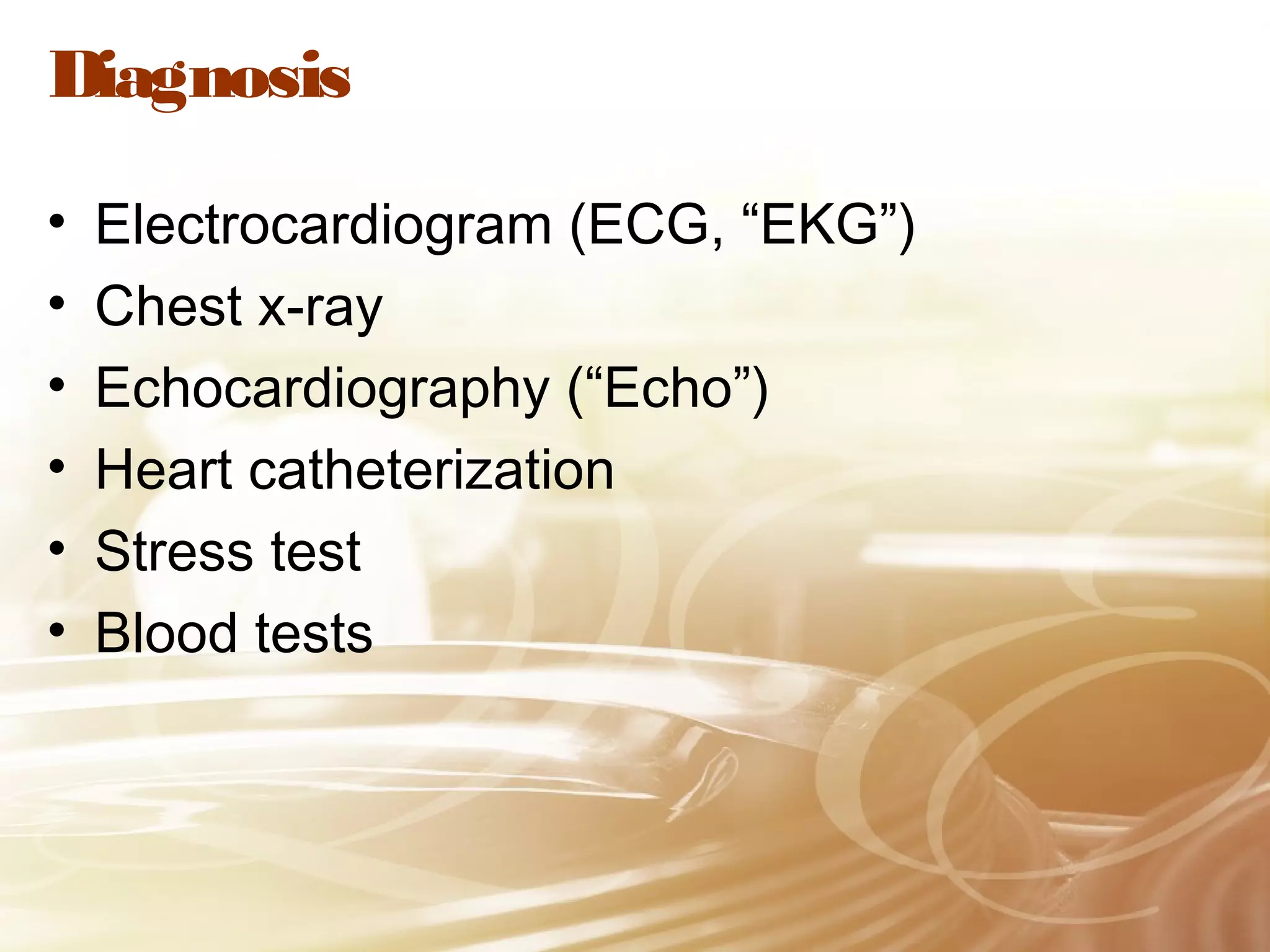
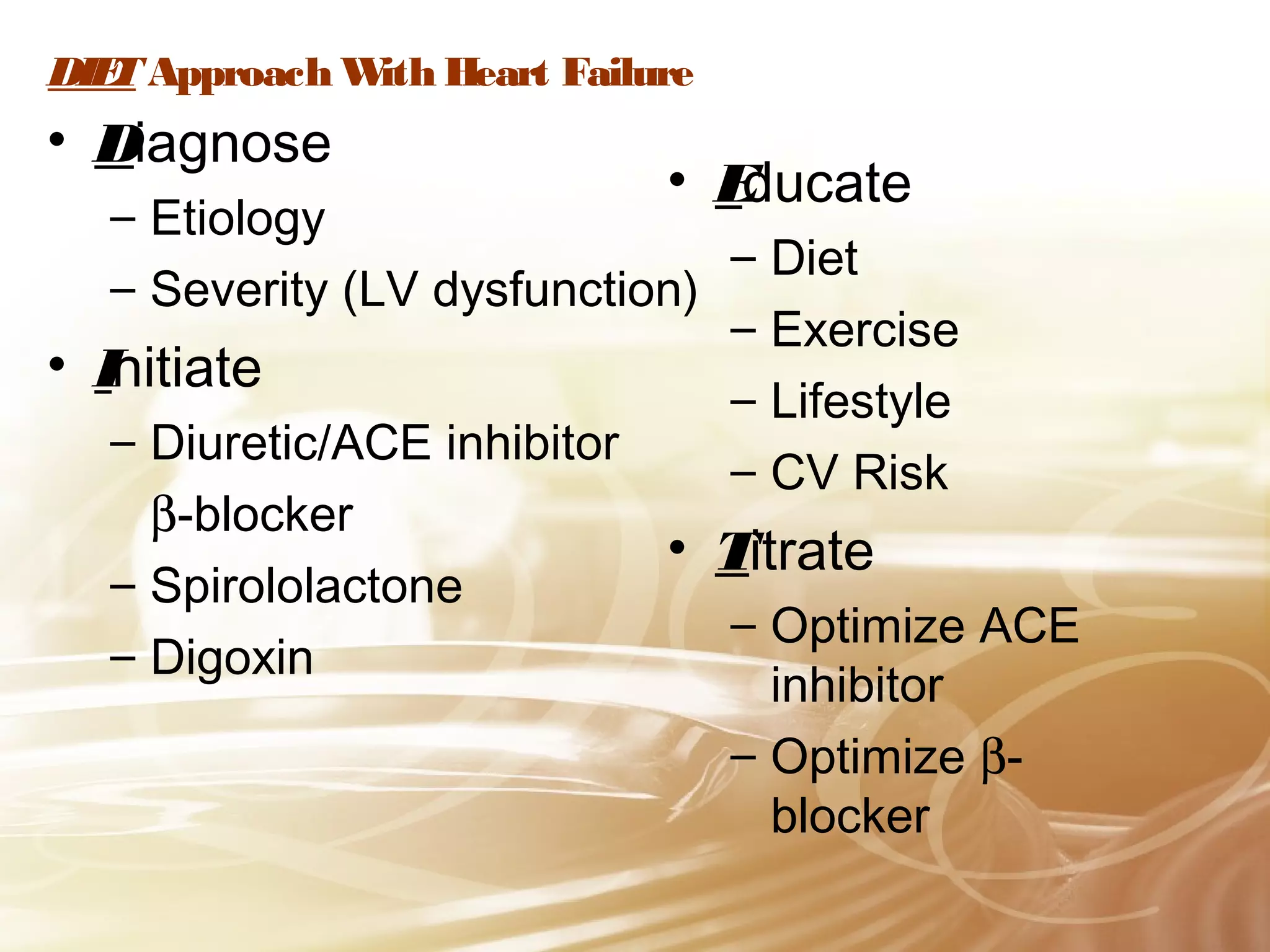
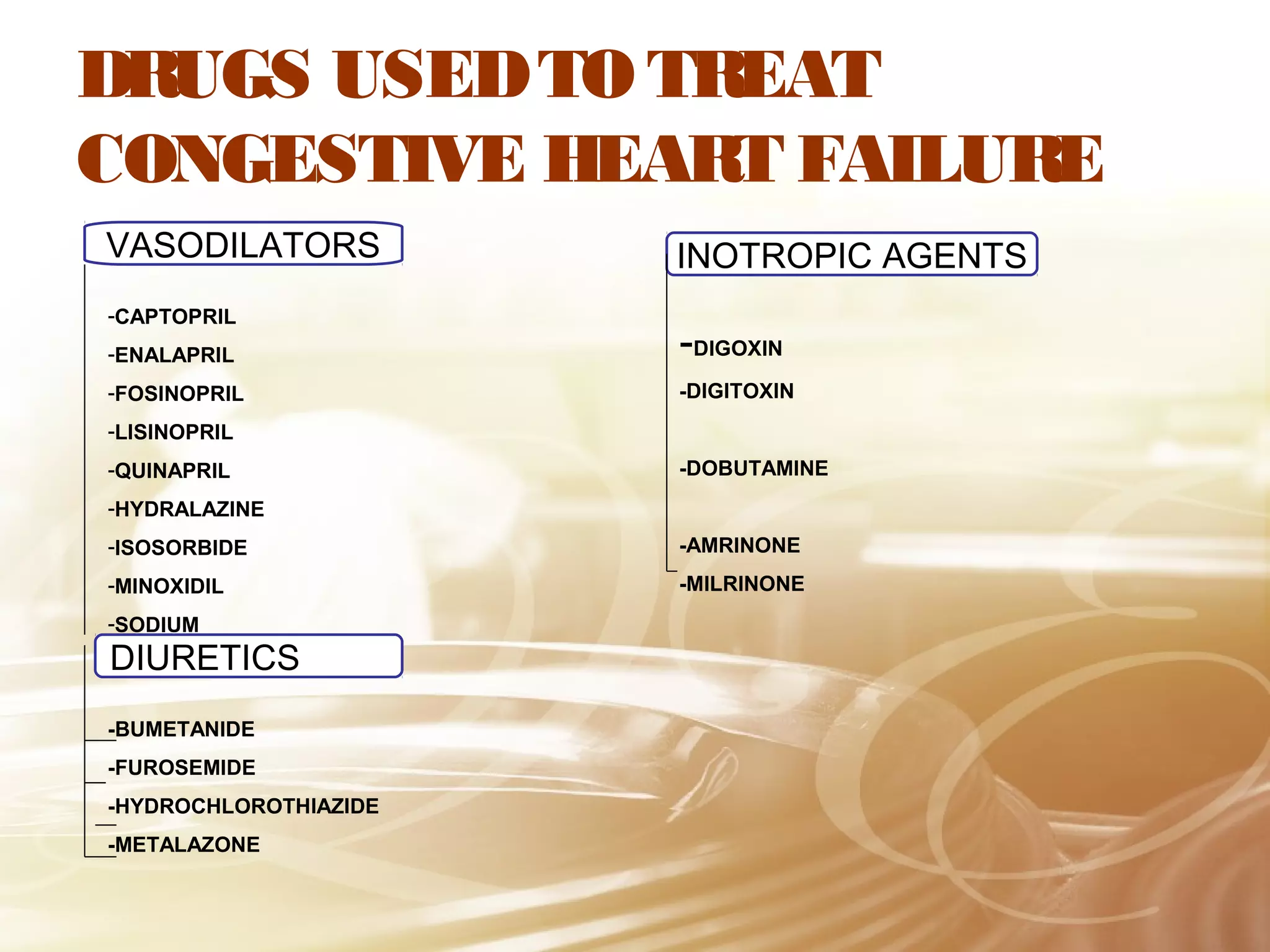
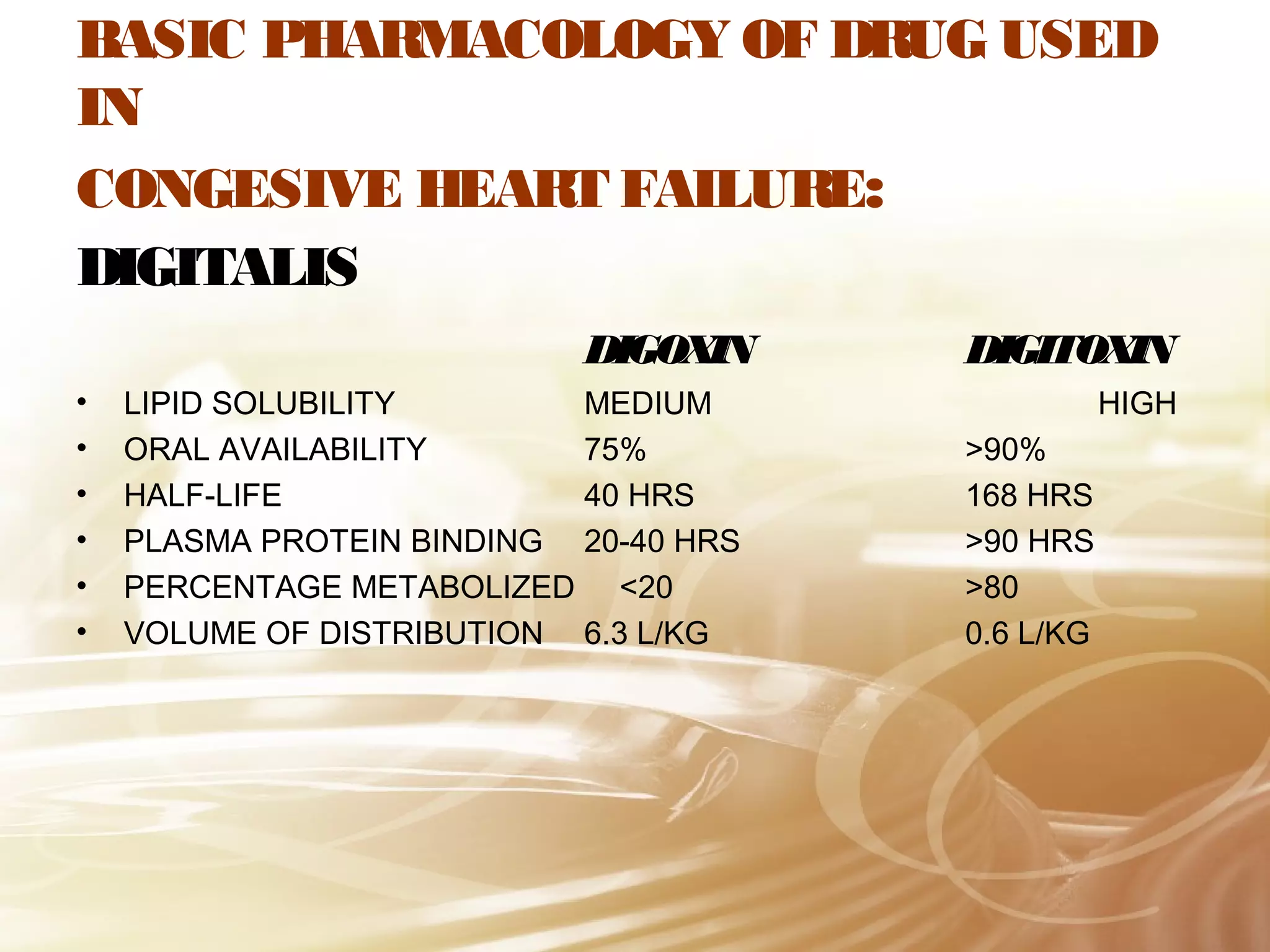
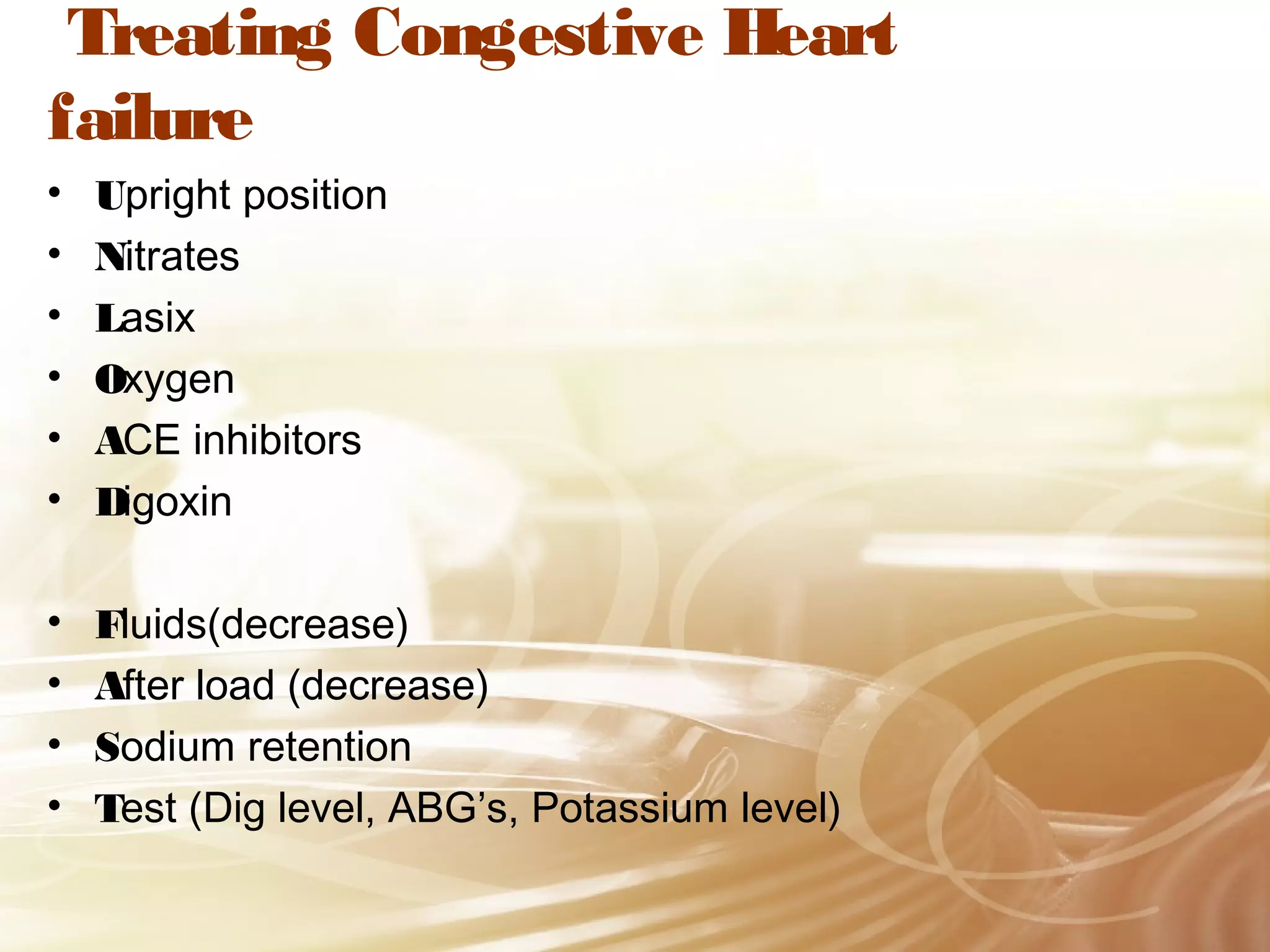
This document provides an overview of congestive heart failure, including its definition, types, causes, symptoms, complications, diagnosis, and treatment. Congestive heart failure occurs when the heart muscle is weakened and cannot pump blood effectively, leading to fluid buildup in tissues and organs. The main types are systolic and diastolic dysfunction. Common causes include hypertension, coronary artery disease, and valvular issues. Symptoms involve fatigue, shortness of breath, and swelling. Treatment focuses on medications like ACE inhibitors, diuretics, beta blockers, and lifestyle changes such as diet, exercise, and stress reduction.