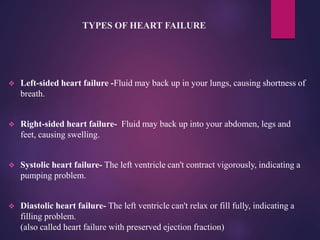
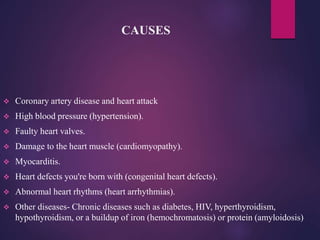
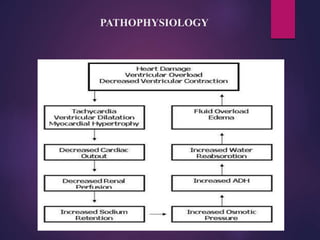
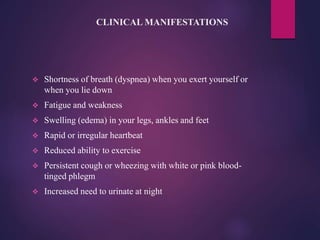
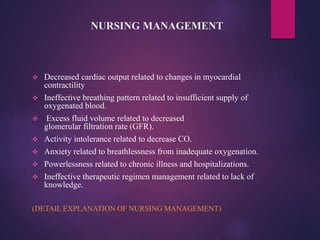
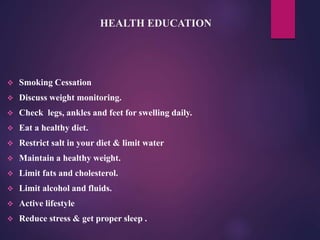
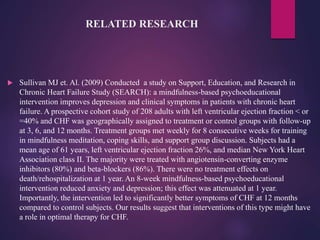
Congestive heart failure is a chronic, progressive condition where the heart cannot pump enough blood to support the organs. It can affect the left or right side of the heart. Risk factors include coronary artery disease, high blood pressure, heart defects, and other chronic diseases like diabetes. Symptoms include shortness of breath, swelling, and fatigue. Diagnosis involves medical history, physical exam, blood tests, electrocardiogram, echocardiogram and other cardiac imaging. Treatment consists of medications to regulate blood pressure and fluid levels, as well as lifestyle changes and potentially surgery. Nursing management focuses on monitoring fluid levels, breathing, and administering medications correctly. Complications can include kidney damage, heart valve problems, and arrhythm