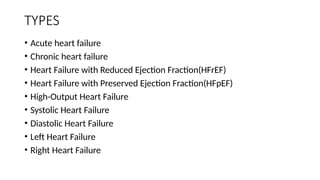
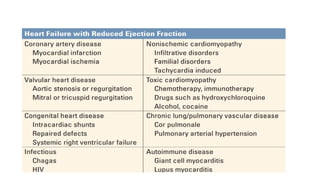
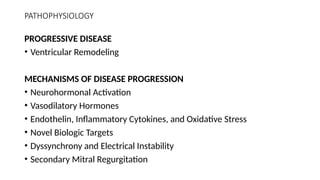
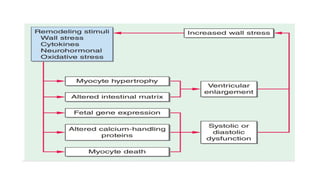
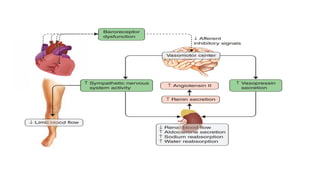
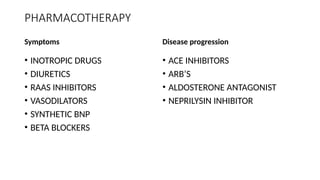
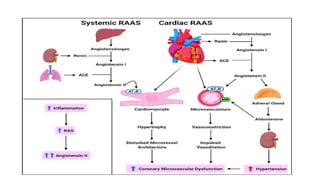
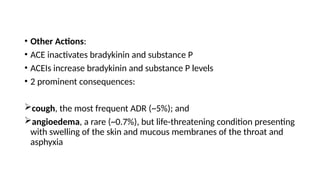
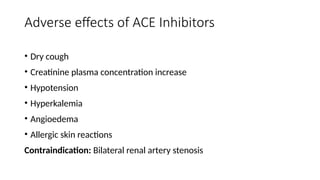
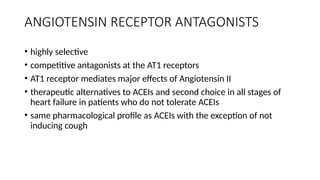
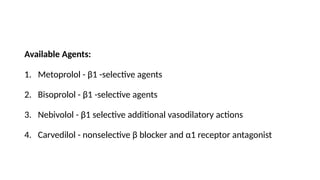
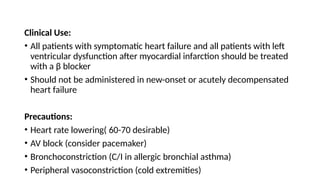
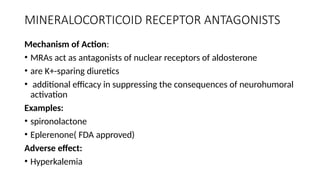
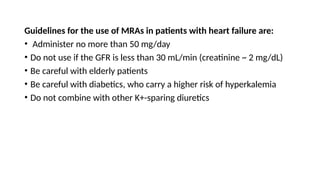
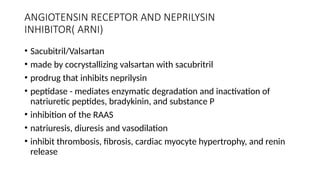
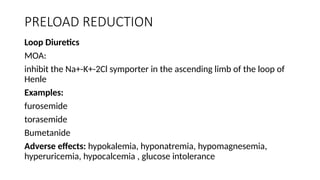
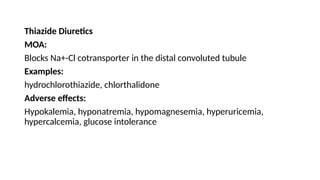
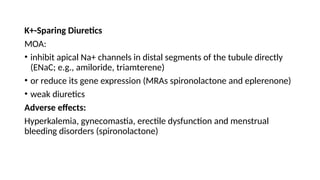
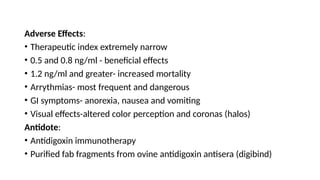
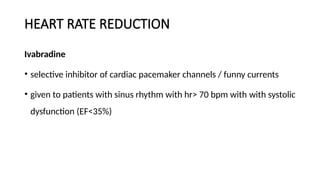
The document provides a comprehensive overview of heart failure, including its definition, types, pathophysiology, symptoms, and pharmacotherapy options. It discusses various medications used in treatment, such as ACE inhibitors, beta blockers, and diuretics, along with their mechanisms of action, adverse effects, and treatment principles. Additionally, it highlights the importance of managing heart failure through neurohumoral modulation, preload and afterload reduction, and increasing cardiac contractility.