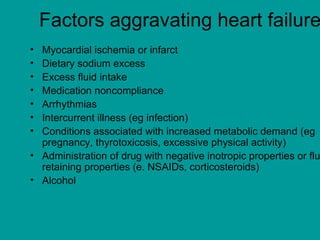
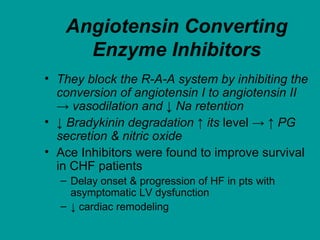
Heart failure is a condition where the heart cannot pump enough blood to meet the body's needs. It has many potential causes, but is often due to problems with the heart muscle itself or valves. Treatment focuses on managing symptoms with diuretics, and slowing progression with ACE inhibitors, beta-blockers, and aldosterone antagonists. Other therapies aim to improve heart function or treat underlying causes. Prognosis depends on severity but ranges from 5-50% annual mortality.