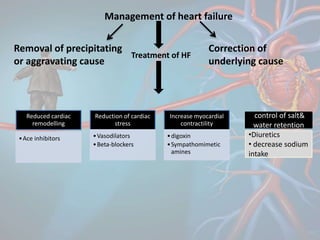
This document provides an overview of heart failure, including its definition, incidence, pathology, types, risk factors, etiology, diagnosis, management, and complications. Some key points:
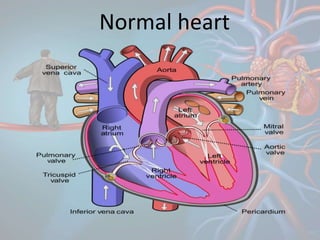
- Heart failure is defined as the heart's inability to pump sufficiently to maintain blood flow to meet the body's needs. It can be acute or chronic and is a common cause of hospitalization.
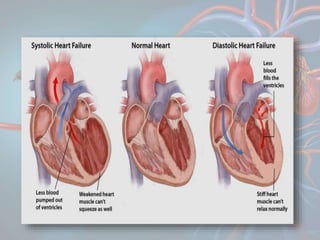
- Pathologically, it involves increases in preload and afterload along with decreased contractility. The main types are based on output (low or high), the ventricles affected (left, right, or both), and systolic or diastolic dysfunction.
- Risk factors include hypertension, diabetes, and coronary artery disease