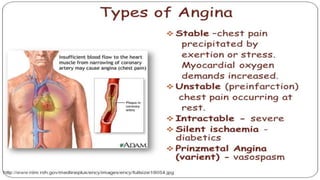
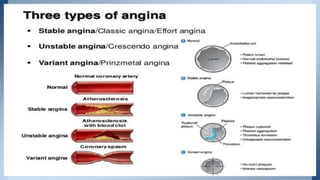
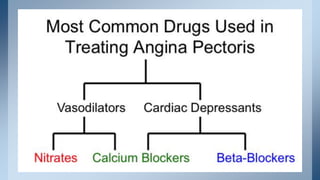
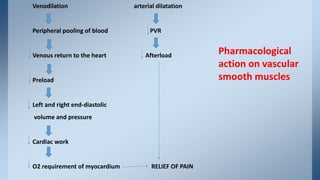
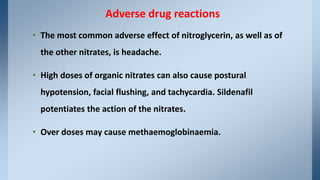
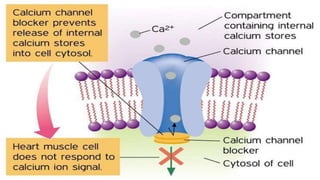
Angina pectoris is a clinical syndrome caused by reduced blood flow to the heart, resulting in transient myocardial ischemia. It presents as chest pain or discomfort that is often exacerbated by exertion or stress. There are three main types - stable angina, unstable angina, and variant angina. Treatment involves lifestyle modifications and medications like nitrates, calcium channel blockers, beta blockers, and antiplatelet drugs to relieve symptoms and reduce cardiac workload.