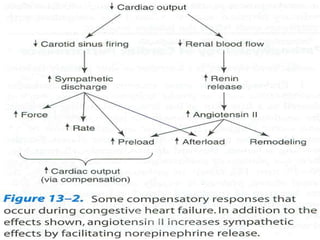
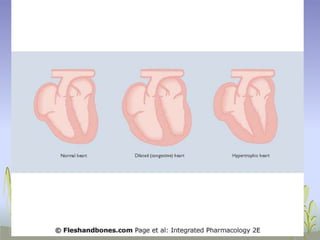
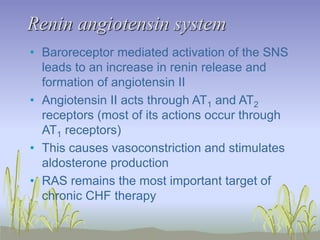
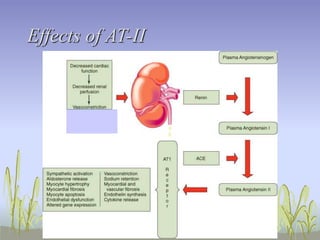
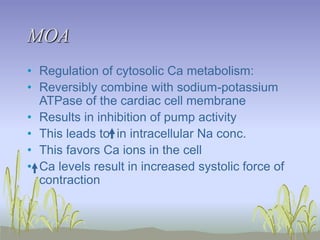
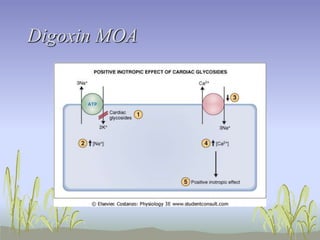
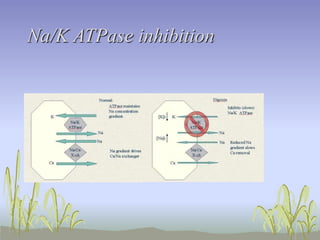
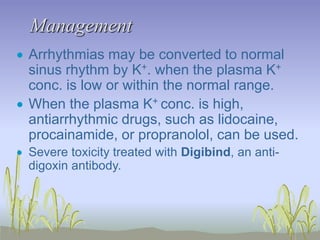
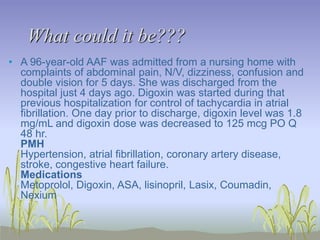
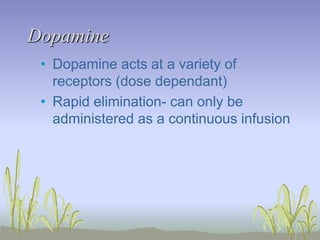
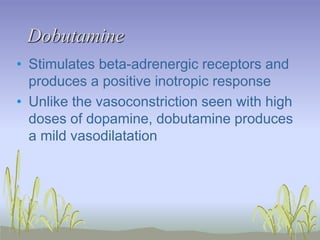
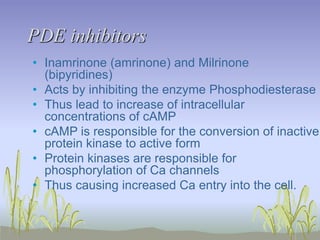
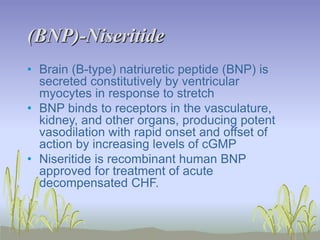
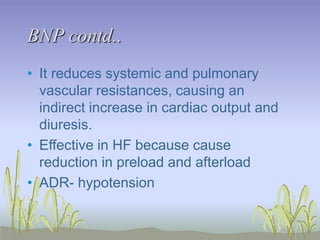
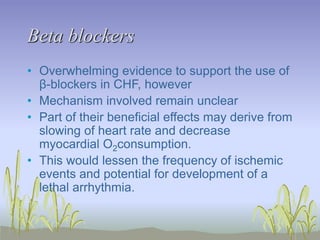
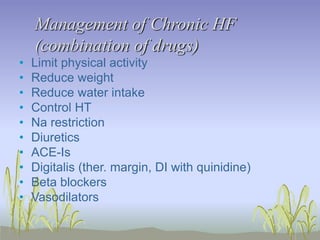
The document provides an extensive overview of congestive heart failure (CHF), highlighting its pathophysiology, management approaches, and treatment options, including both drug and non-drug therapies. It emphasizes the complexity of CHF, addressing the roles of the sympathetic nervous system and the renin-angiotensin-aldosterone system, while discussing the implications of advanced therapies and recent research findings. Additionally, the document outlines the significance of managing symptoms, improving quality of life, and decreasing mortality in patients with heart failure.