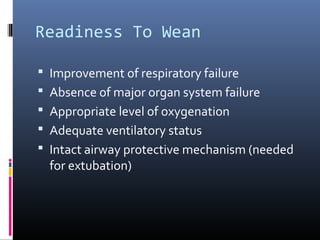
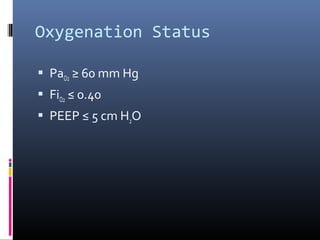
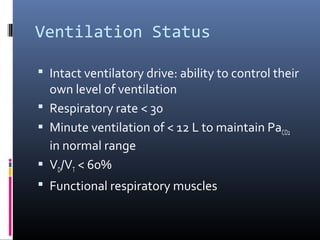
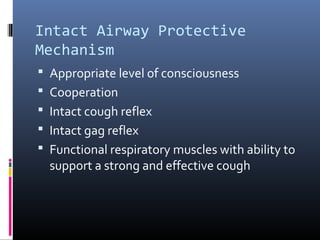
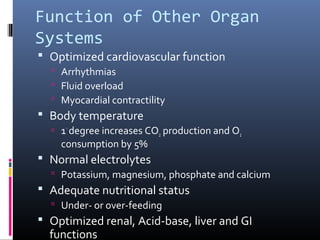
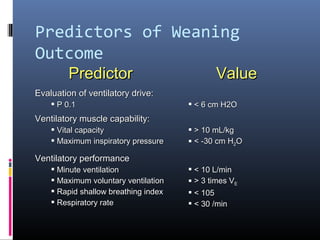
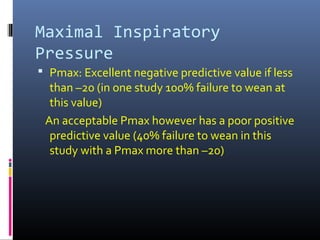
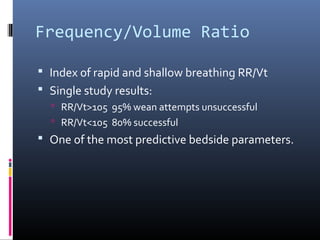
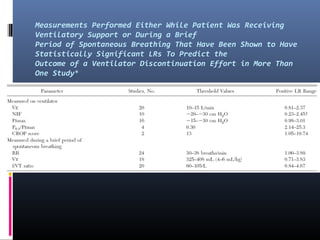
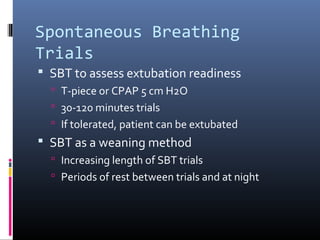
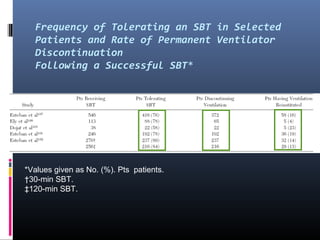
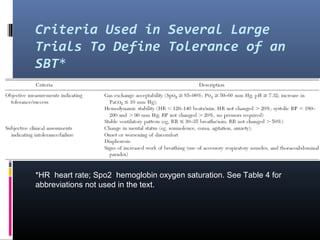
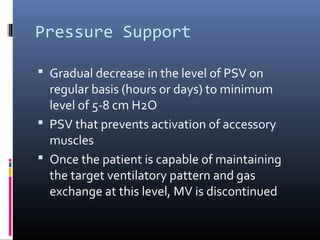
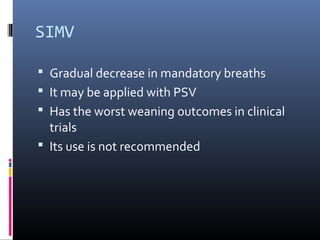
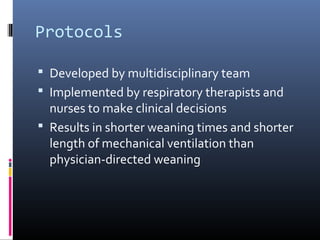
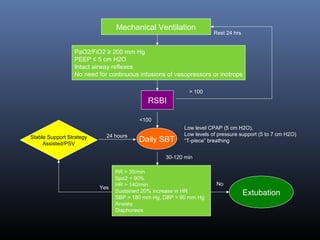
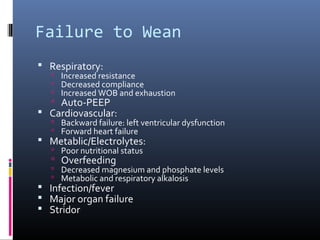
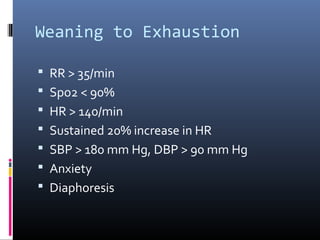
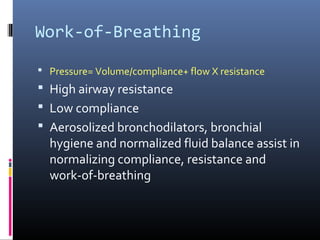
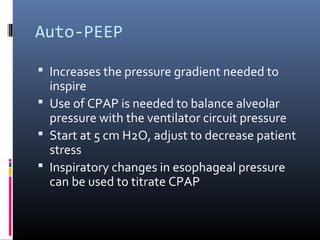
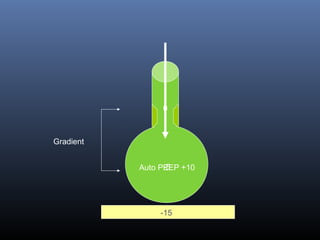
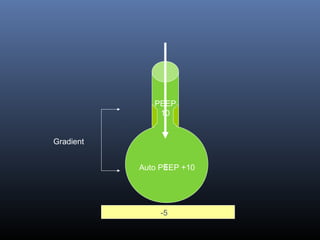
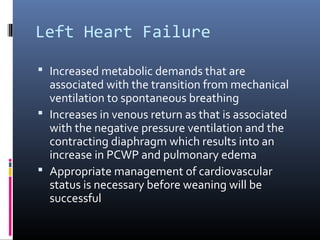
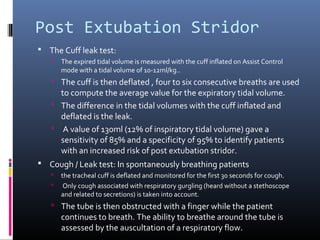
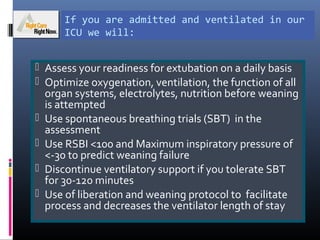
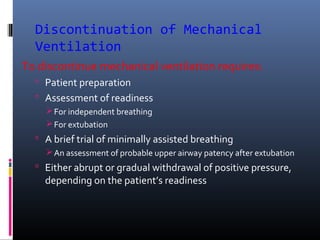
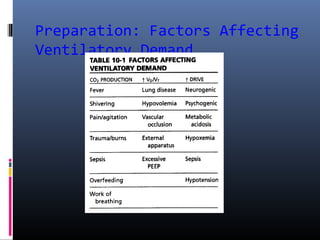
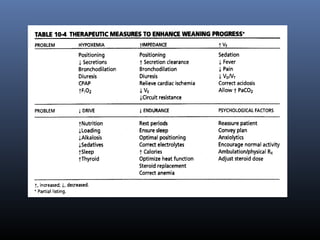
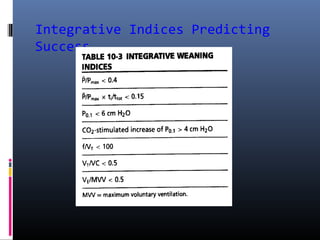
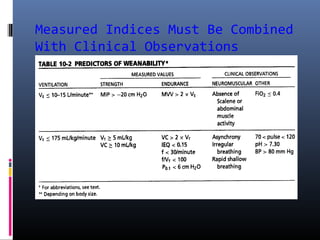
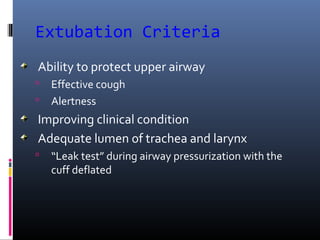
This document discusses strategies for liberating patients from mechanical ventilation. It outlines key factors that indicate readiness to wean, including improved respiratory function and organ system stability. Two common approaches to weaning are described: gradual weaning using methods like pressure support ventilation or spontaneous breathing trials followed by extubation if tolerated. Protocols using objective criteria can standardize and expedite the weaning process. Factors that may cause weaning failure include respiratory issues, cardiovascular problems, or infection. Readiness is assessed through measurements of ventilatory drive, muscle strength, and breathing patterns.