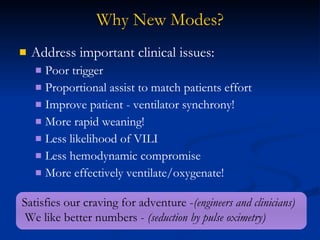
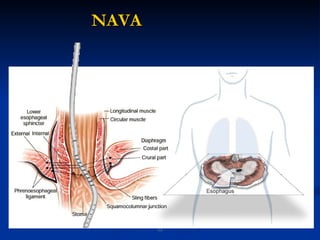
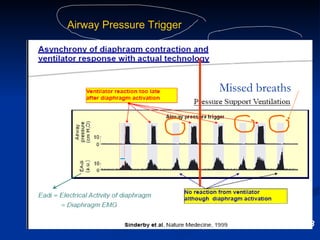
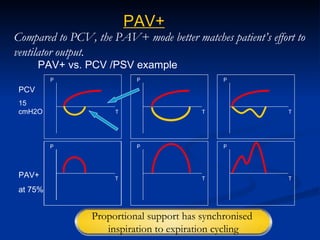
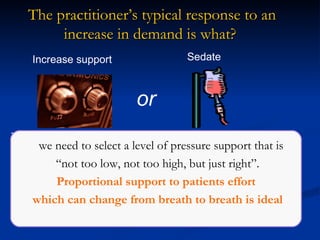
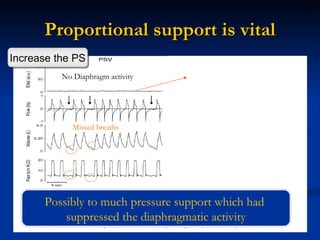
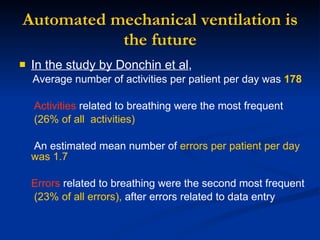
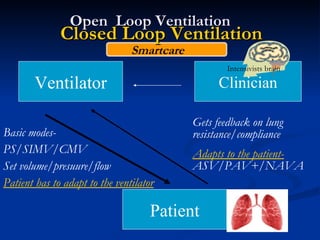
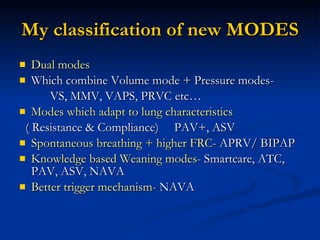
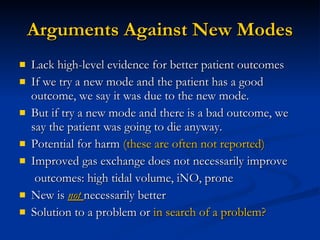
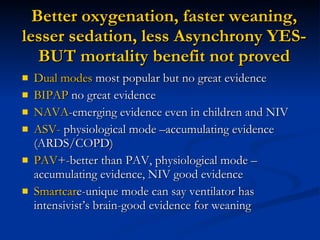
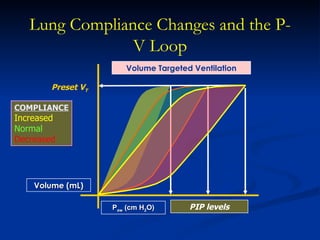
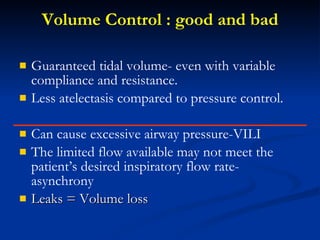
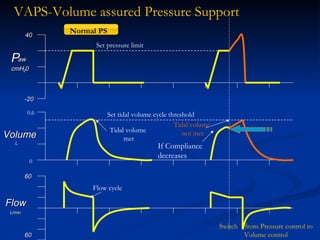
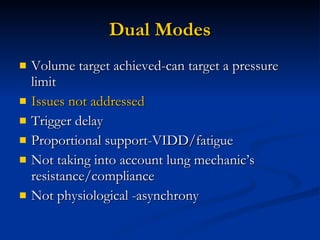
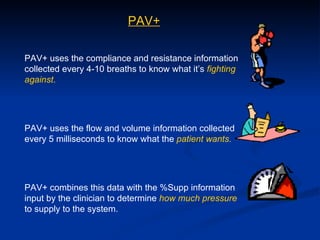
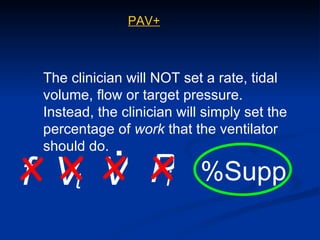
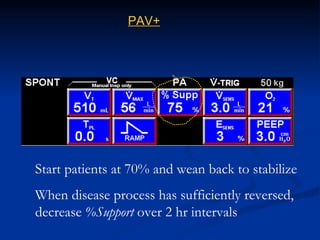
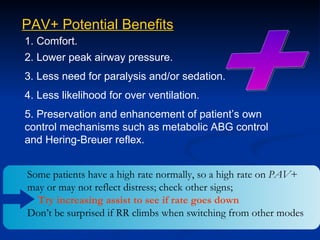
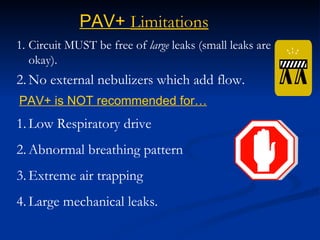
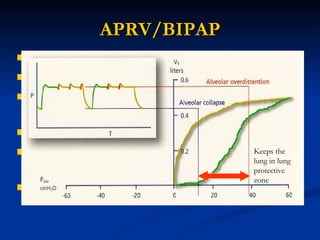
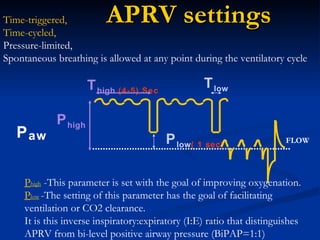
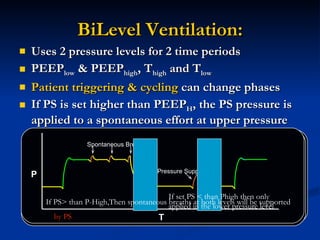
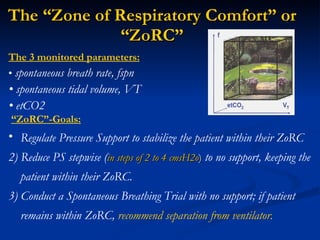
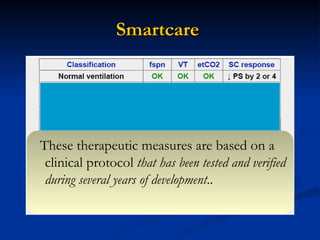
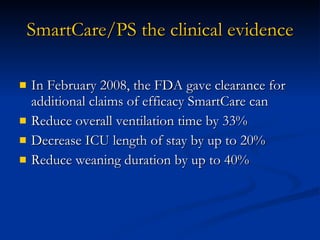
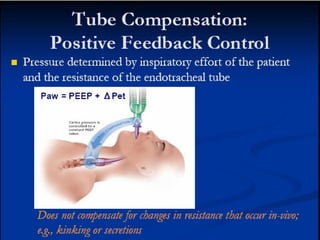
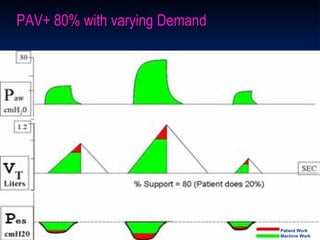
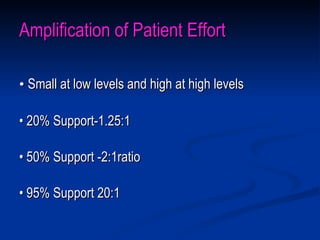
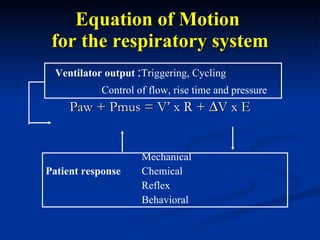
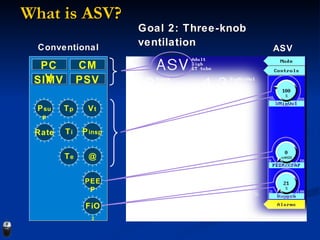
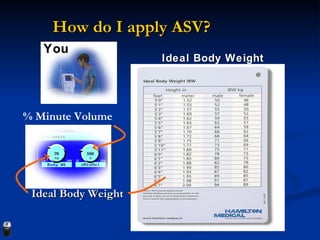
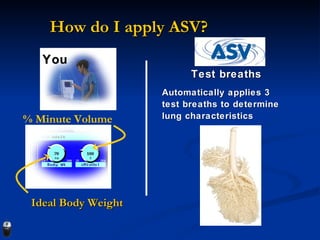
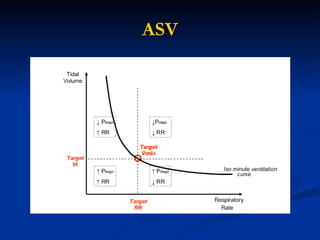
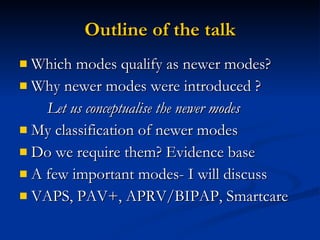
The document discusses newer modes of mechanical ventilation that were introduced to address clinical issues like poor patient-ventilator synchrony, prolonged weaning times, and ventilator-induced lung injury. It classifies the newer modes as dual modes that combine volume and pressure control, modes that adapt to lung characteristics, and knowledge-based weaning modes. It provides more details on proportional assist ventilation (PAV+), airway pressure release ventilation (APRV/BIPAP), and Smartcare—modes that aim to improve synchrony, maintain high functional residual capacity, and reduce workload for clinicians respectively.
![SIMV PCV ACV CMV Basic Modes? PS Newer [Alternative] Modes ? Volume support (VS) Volume Assured Pressure Support (VAPS) Pressure regulated volume control ventilation (PRVC) Mandatory minute ventilation (MMV) PROPORTIONAL ASSIST VENTILATION(PAV) ADAPTIVE SUPPORT VENTILATION(ASV) Smartcare/Automatic tube Compensation BIPAP/DUOPAP Airway pressure release ventilation (APRV ) High Frequency Ventilation/oscillation Partial Liquid Ventilation (Perflurocarbon) Neurally Adjusted Ventilatory Assist (NAVA) Fractal ventilation](https://image.slidesharecdn.com/newmodesofmechanicalventilationtrc-100815080249-phpapp02/85/New-modes-of-mechanical-ventilation-TRC-3-320.jpg)