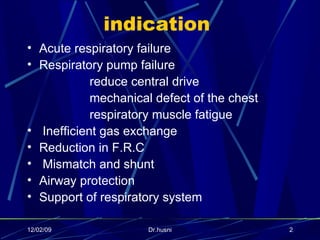
The document discusses various topics related to mechanical ventilation including:
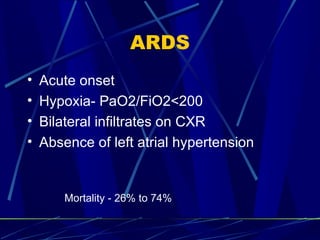
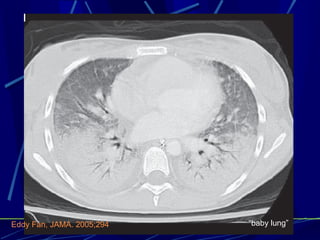
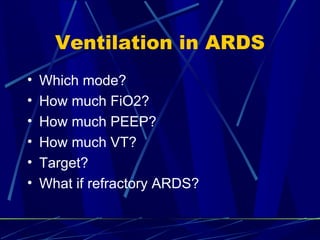
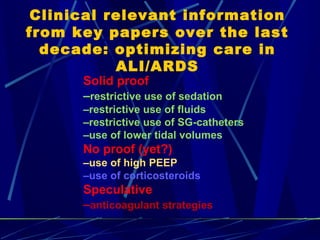
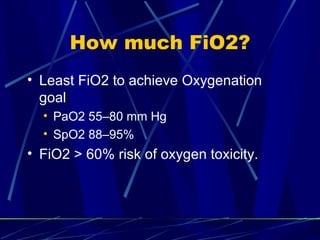
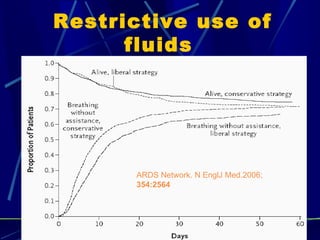
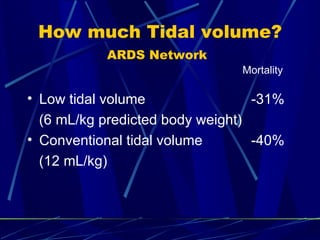
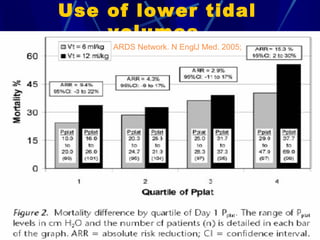
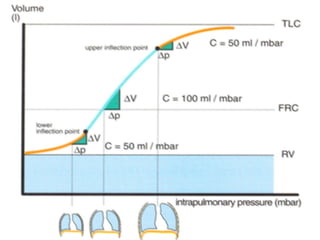
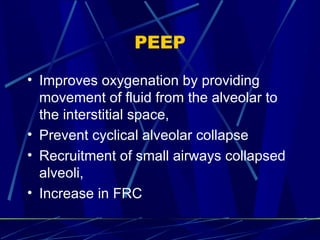
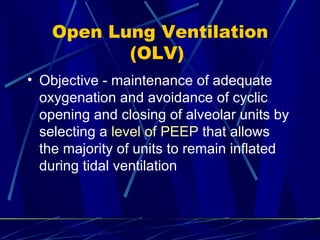
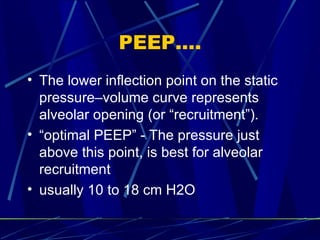
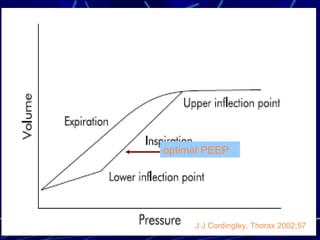
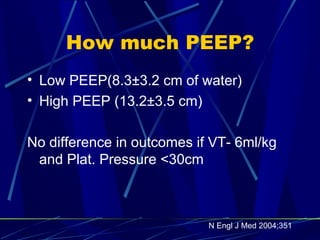
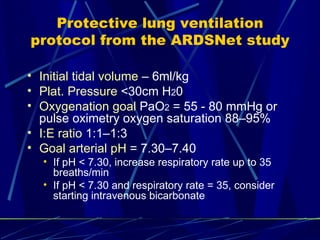
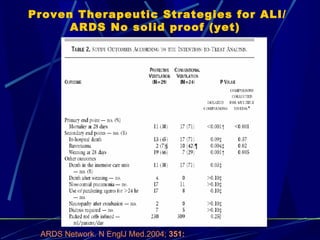
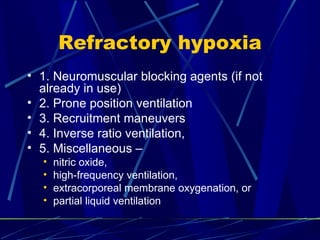
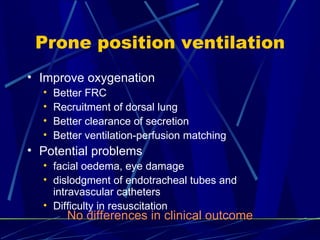
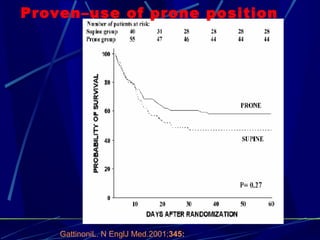
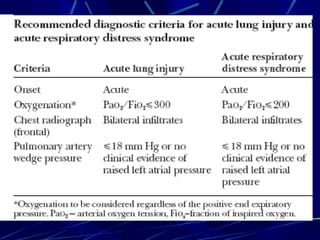
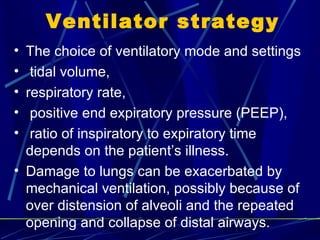
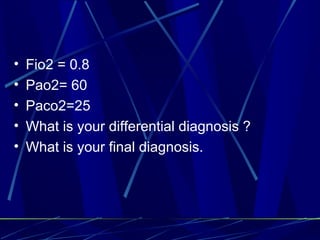
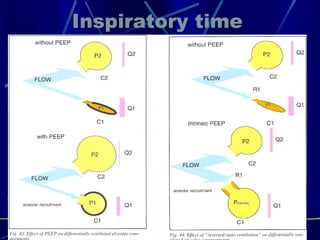
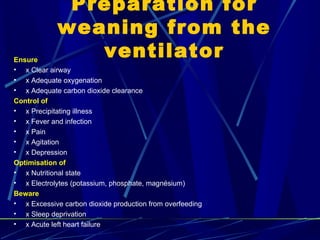
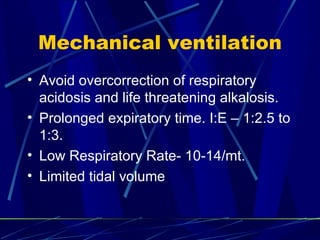
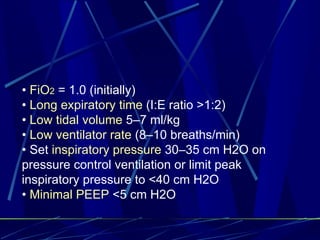
1. Ventilation strategies for acute respiratory distress syndrome (ARDS) including low tidal volumes, optimal positive end-expiratory pressure, and prone positioning.
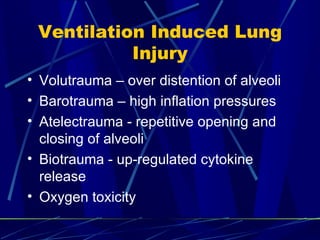
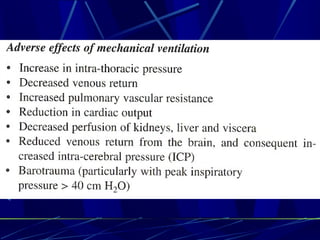
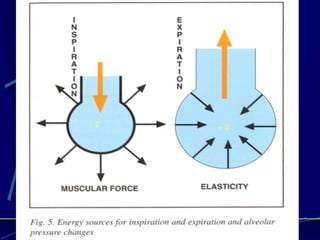
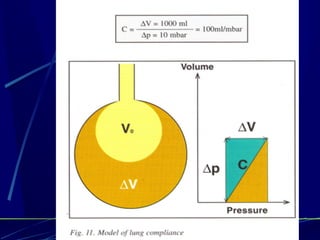
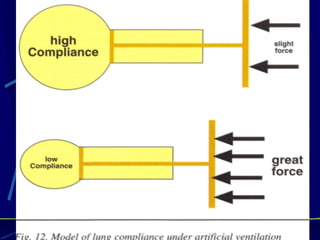
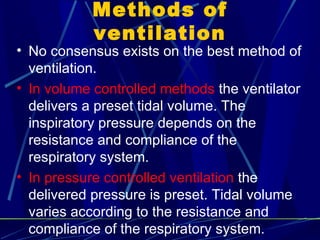
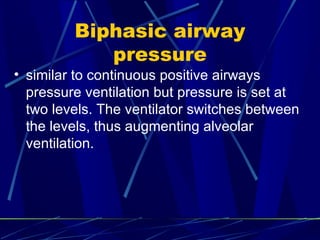
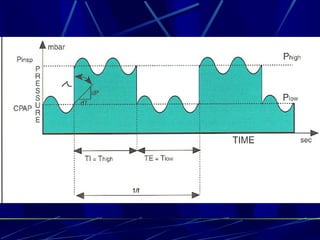
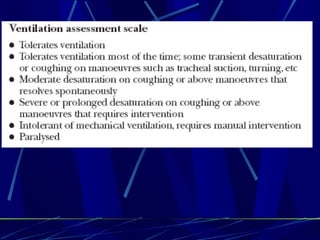
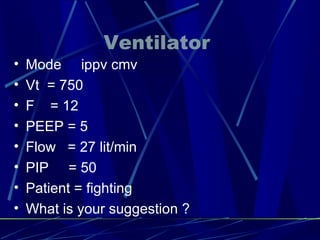
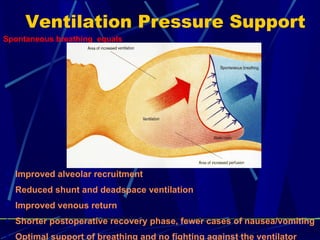
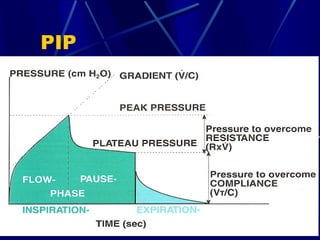
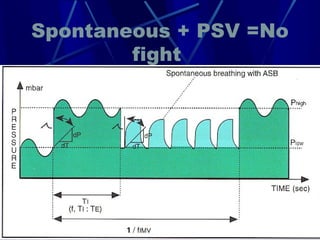
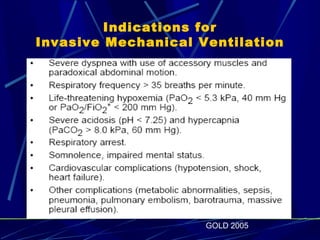
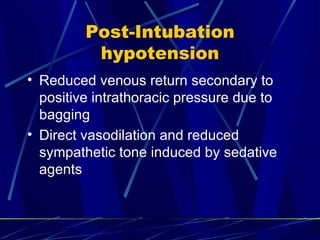
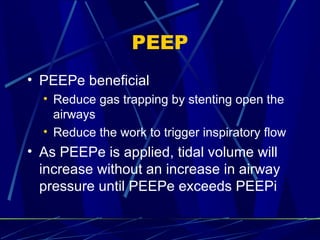
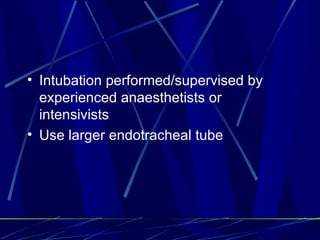
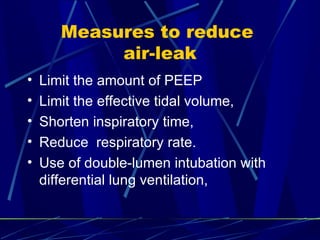
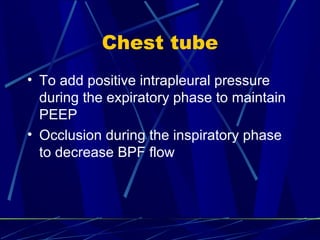
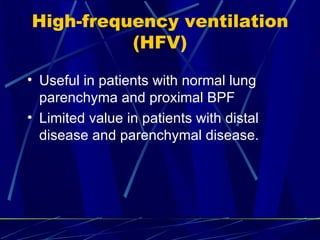
2. Ventilation modes and settings should be tailored to the individual patient's condition and aim to prevent ventilator-induced lung injury.
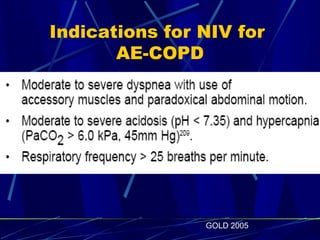
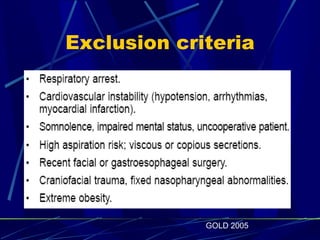
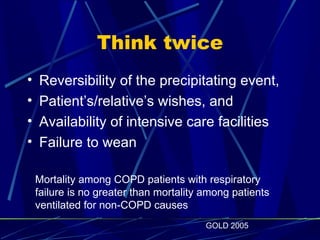
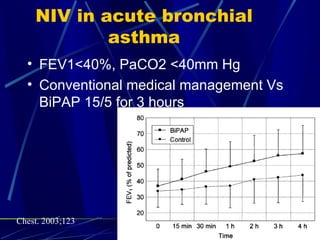
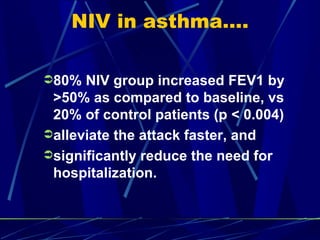
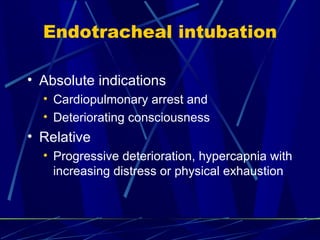
3. Non-invasive ventilation can be considered for certain patients with COPD or asthma to avoid intubation if criteria are met.