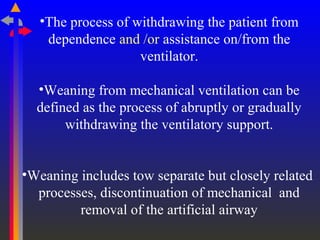
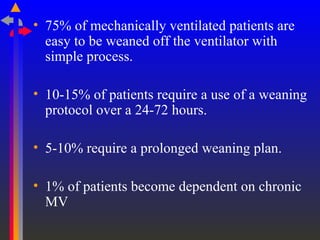
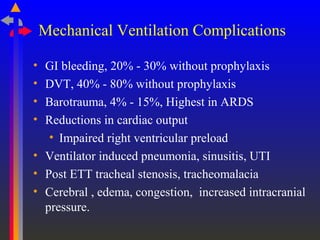
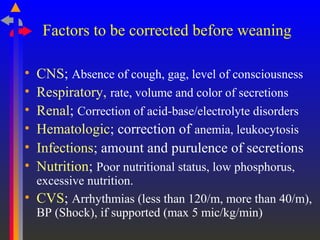
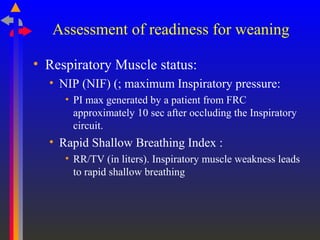
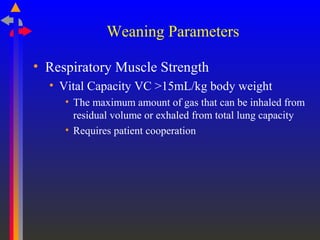
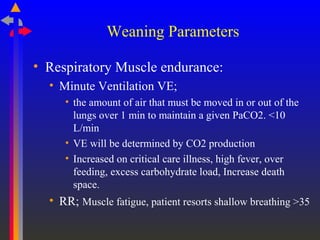
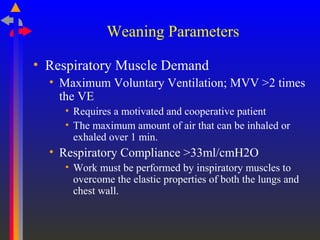
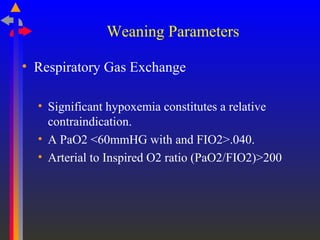
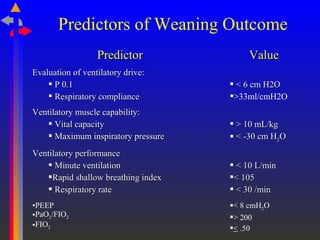
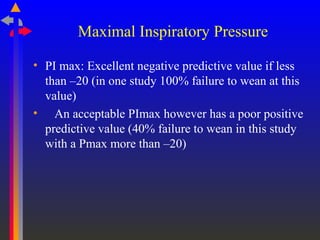
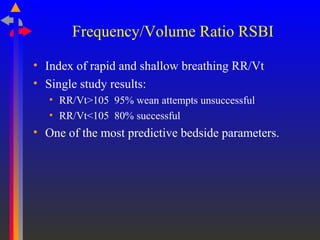
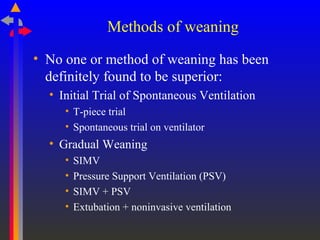
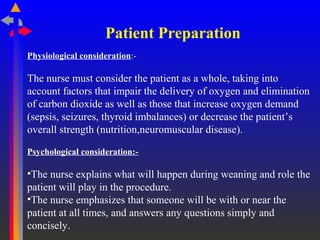
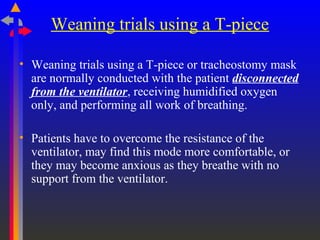
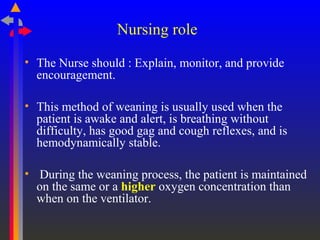
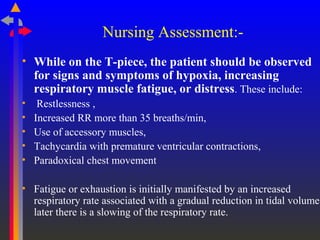
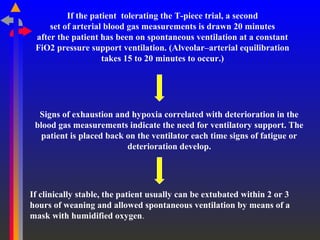
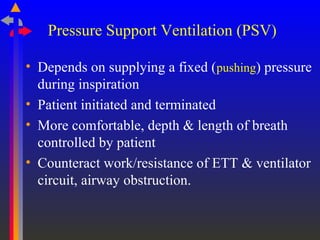
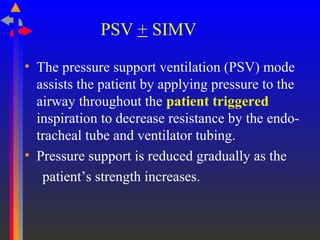
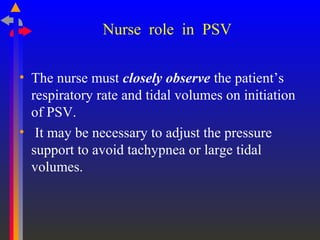
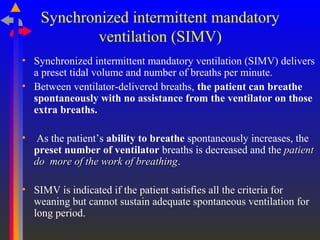
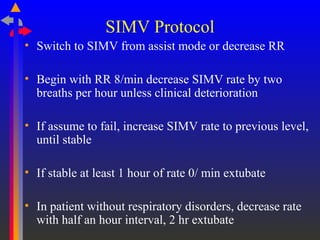
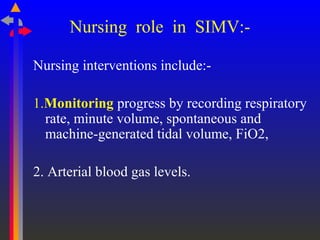
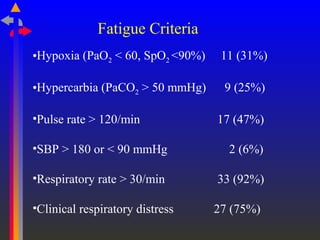
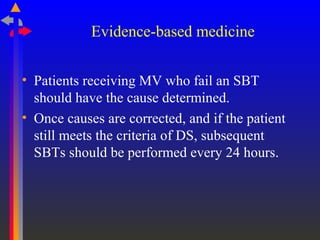
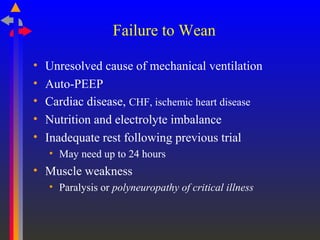
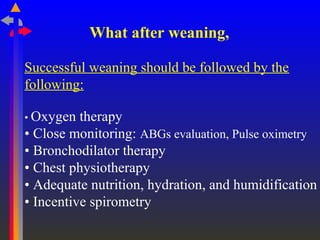
The document discusses weaning patients from mechanical ventilation. It defines weaning as the process of withdrawing ventilator support and describes the main steps as assessing patient readiness, using methods like a T-piece trial or pressure support ventilation to gradually reduce support, and monitoring for signs of fatigue or deterioration. Key factors that must be evaluated for readiness include respiratory muscle strength and endurance, ventilatory drive, gas exchange, and hemodynamic status. Nursing plays an important role in explaining the process, monitoring patients, and providing encouragement during weaning trials.