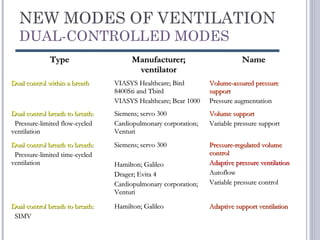
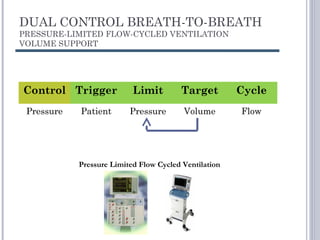
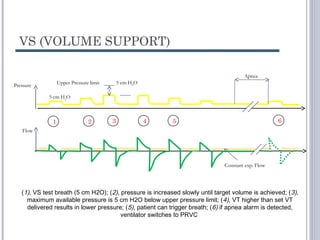
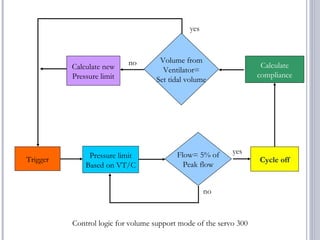
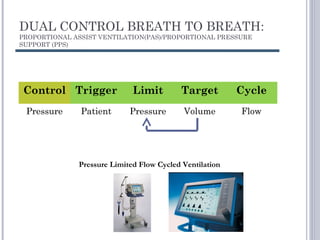
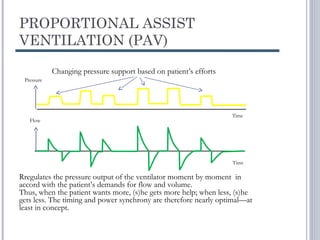
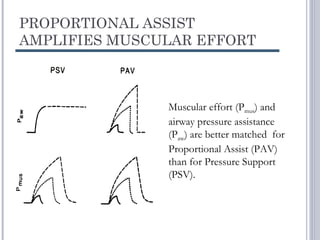
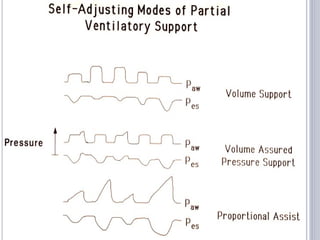
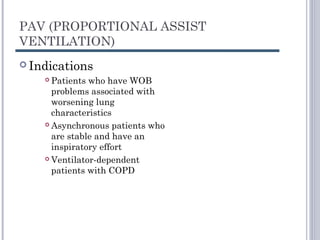
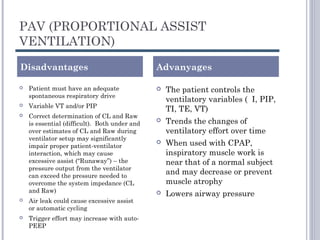
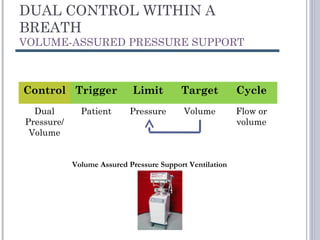
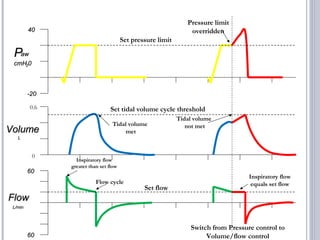
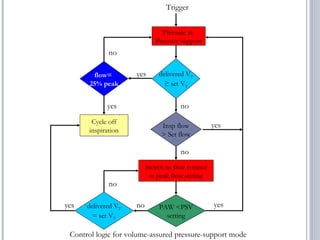
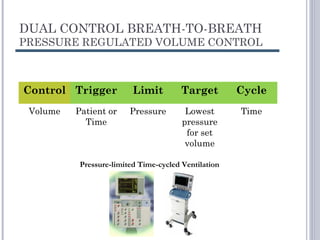
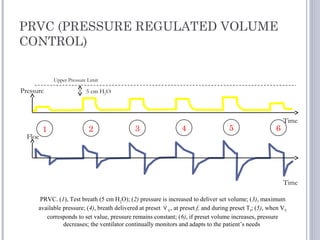
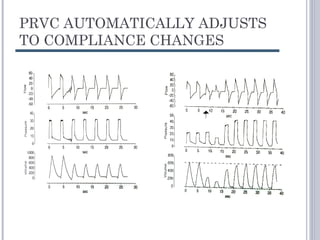
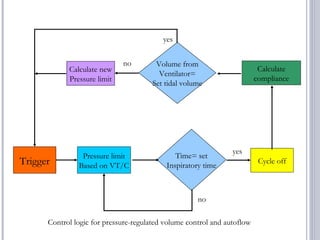
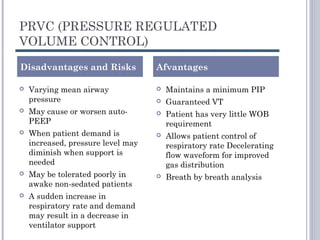
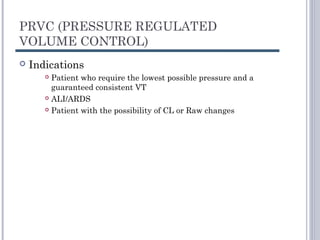
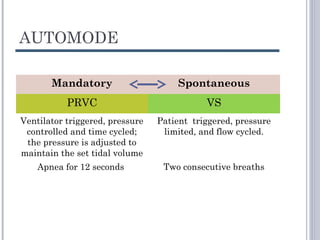
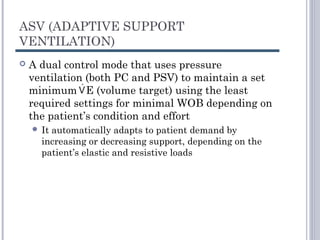
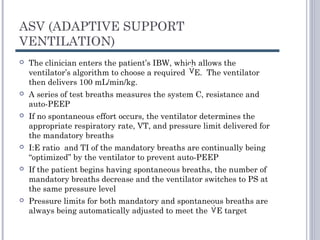
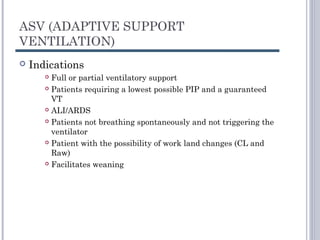
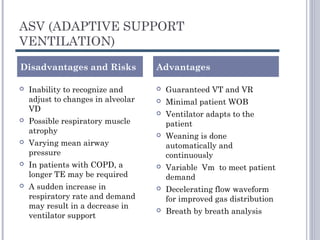
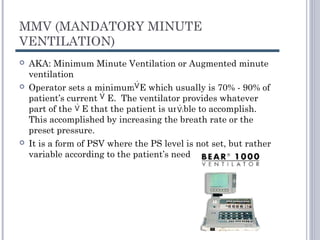
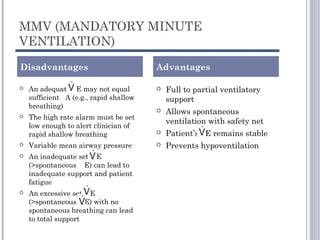
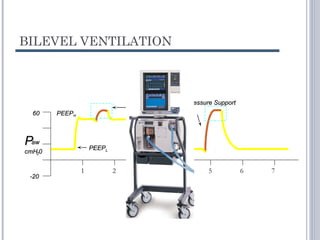
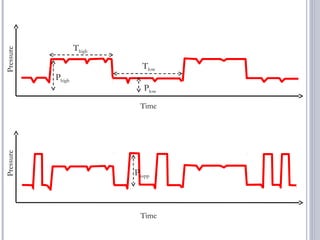
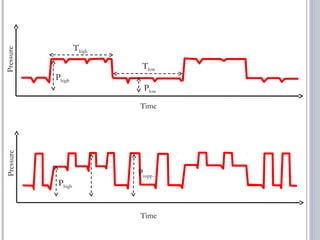
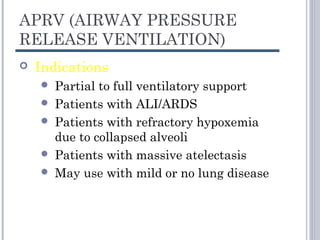
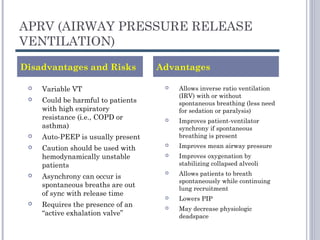
This document discusses several advanced modes of mechanical ventilation. It begins by describing triggered modes like volume support (VS) and proportional assist ventilation (PAV) which provide pressure support that varies based on patient effort. It then covers hybrid modes like volume-assured pressure support and pressure regulated volume control (PRVC) which use dual controls. Newer dual-controlled modes are presented that regulate pressure and volume both within and between breaths. Modes like adaptive support ventilation (ASV) automatically adapt settings to patient changes. Pros, cons and indications are provided for some of the more complex modes.