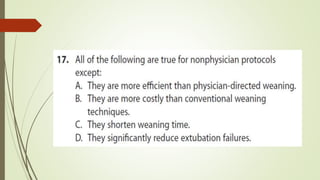
The document discusses guidelines and recommendations for weaning patients from mechanical ventilation and discontinuing ventilator support. Some key points covered include:
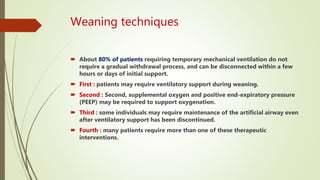
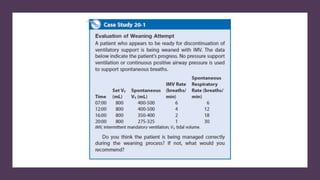
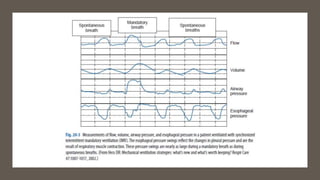
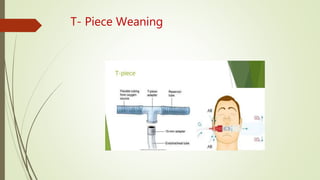
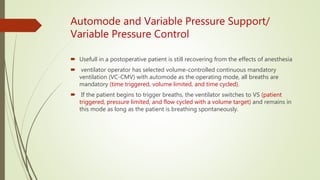
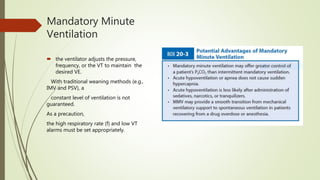
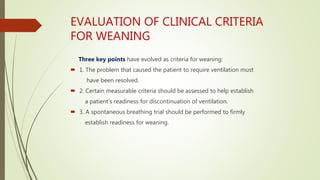
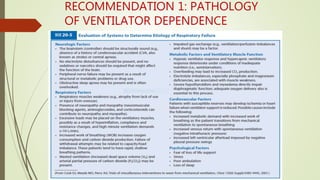
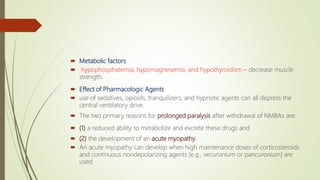
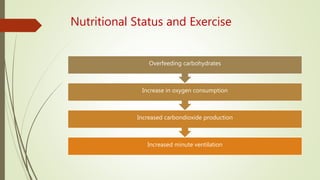
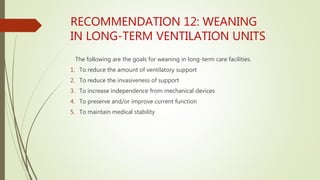
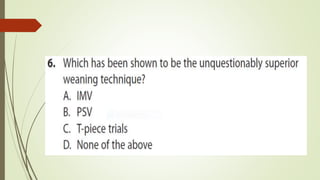
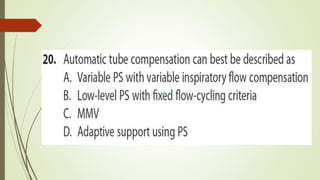
- Weaning involves gradually reducing ventilatory support as a patient's condition improves to avoid complications of prolonged ventilation.
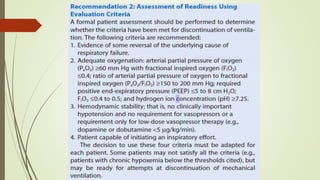
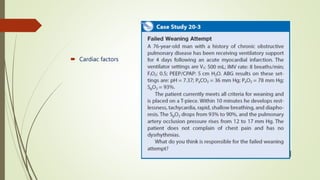
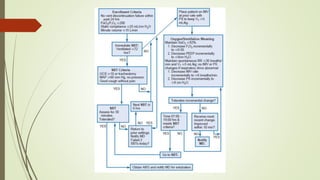
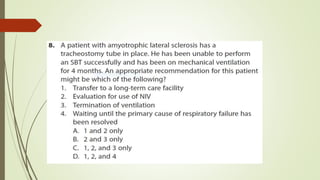
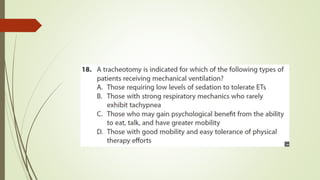
- Readiness for weaning depends on recovery from the underlying medical issues, overall clinical condition, and psychological state.
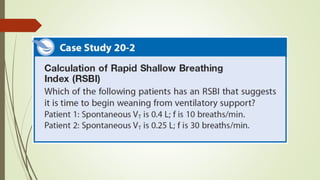
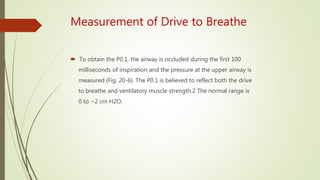
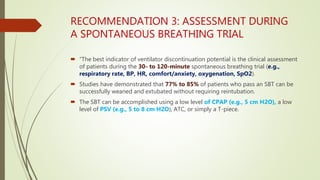
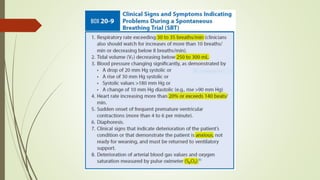
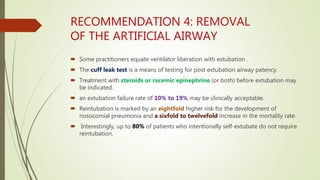
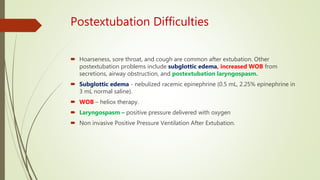
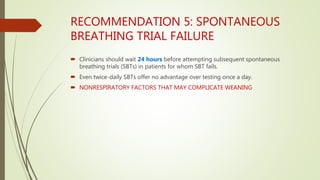
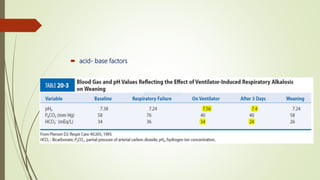
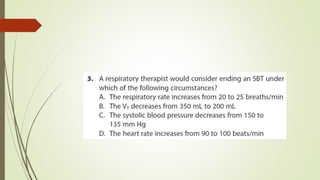
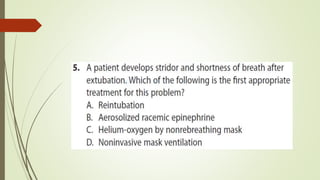
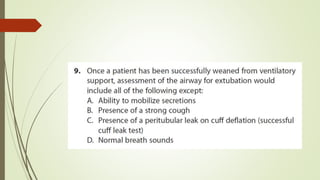
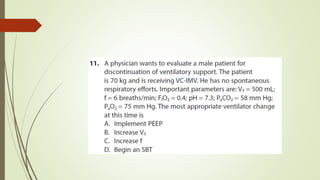
- Spontaneous breathing trials are recommended to assess a patient's ability to breathe independently without ventilator support.
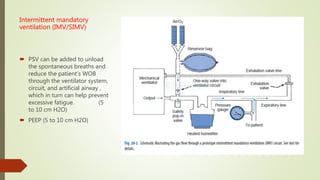
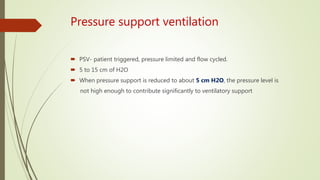
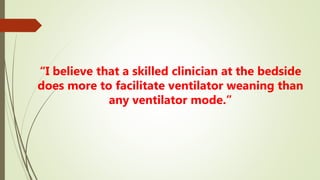
- Factors like ventilator mode, oxygen needs, airway protection, and non-respiratory medical conditions must be considered during the weaning process.
- Protocols and guidelines aim to standard