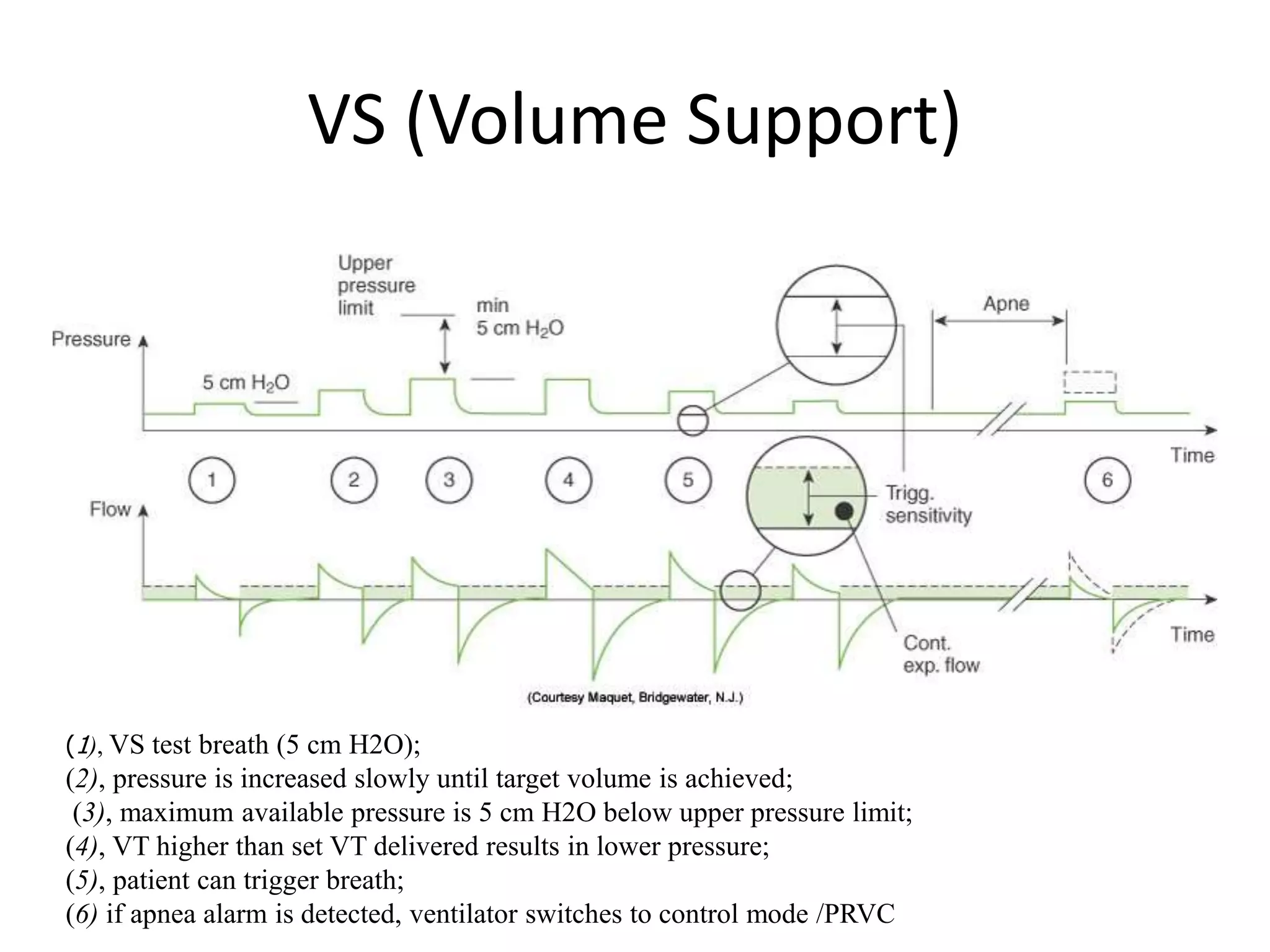
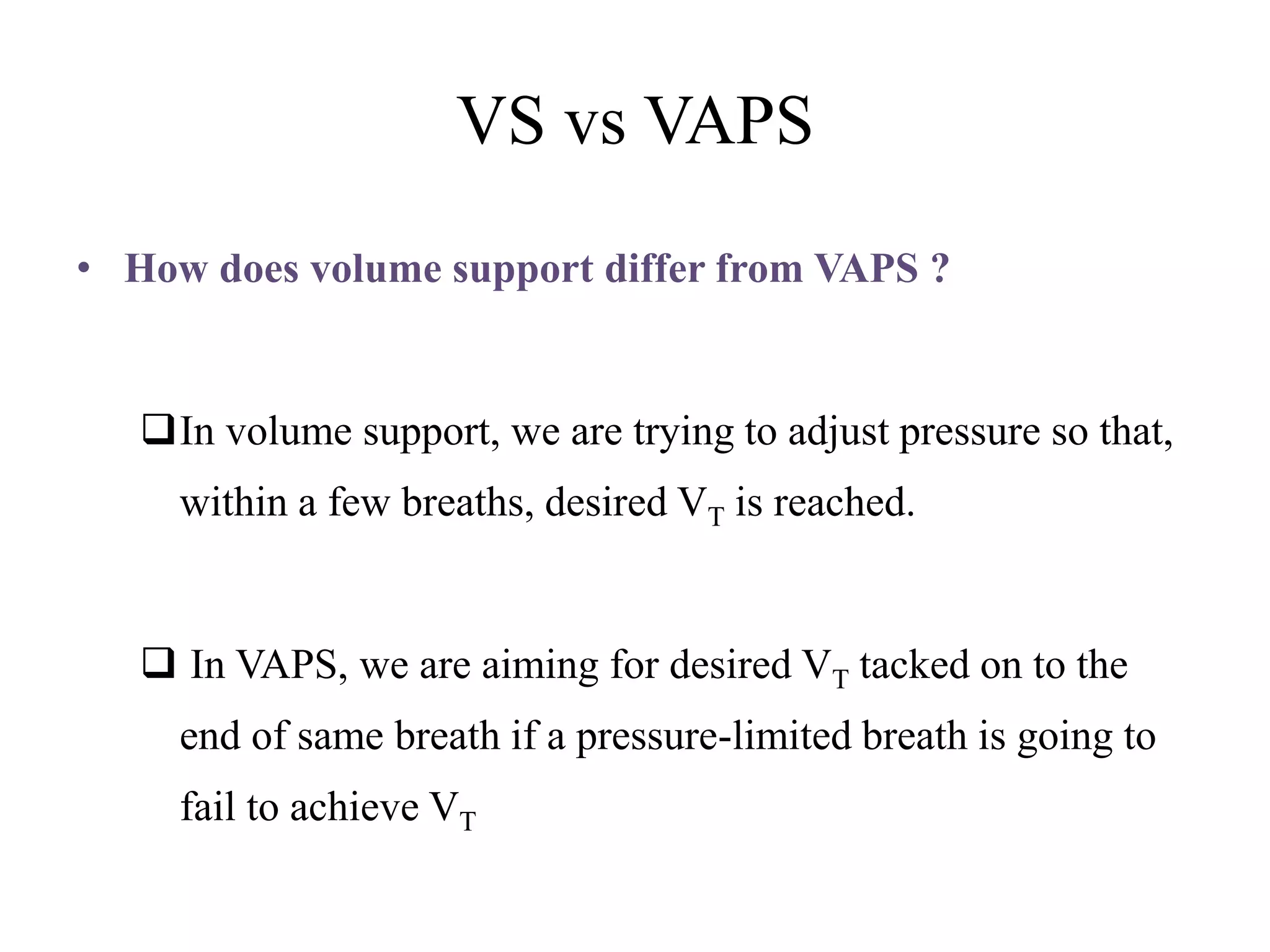
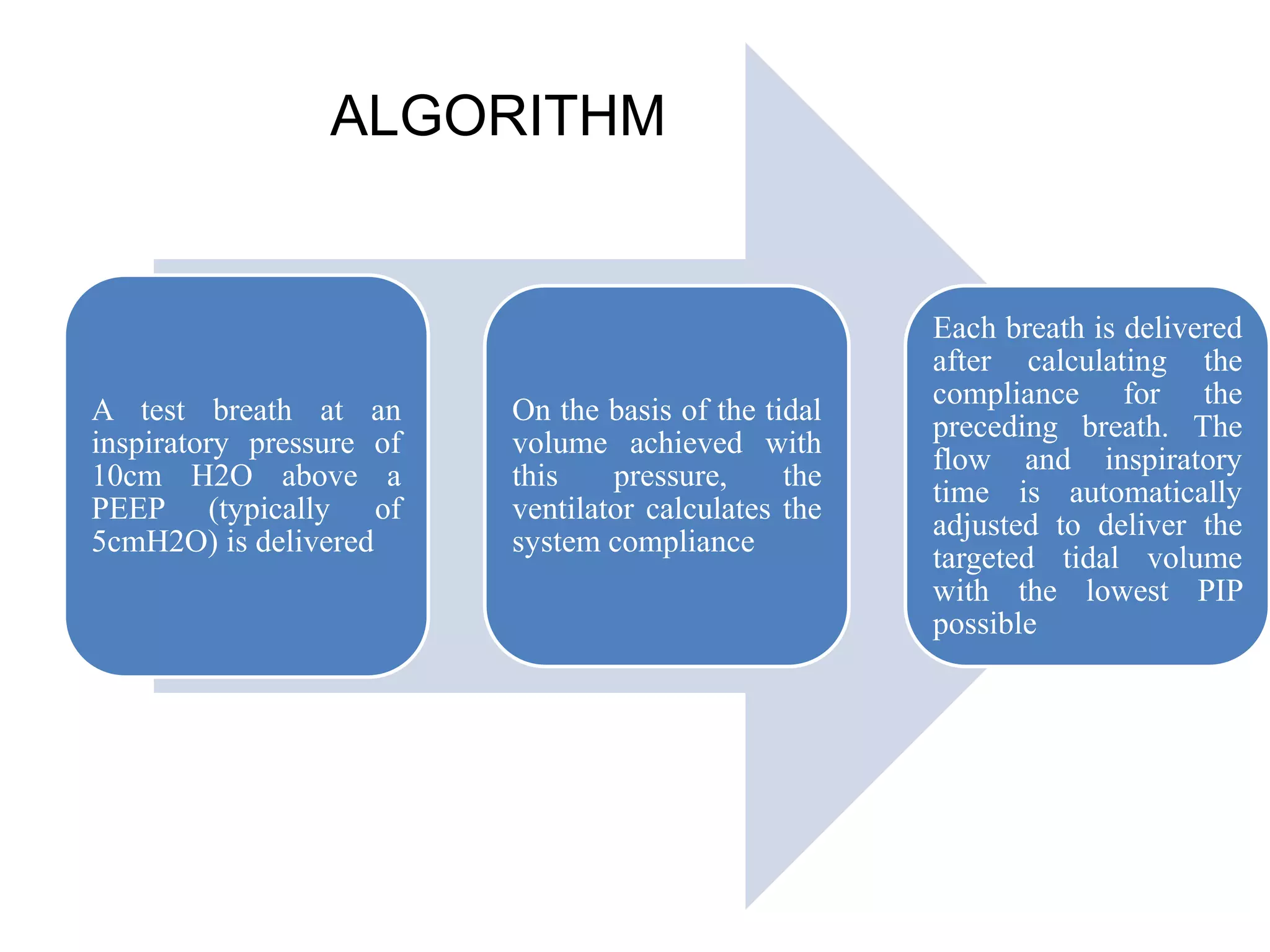
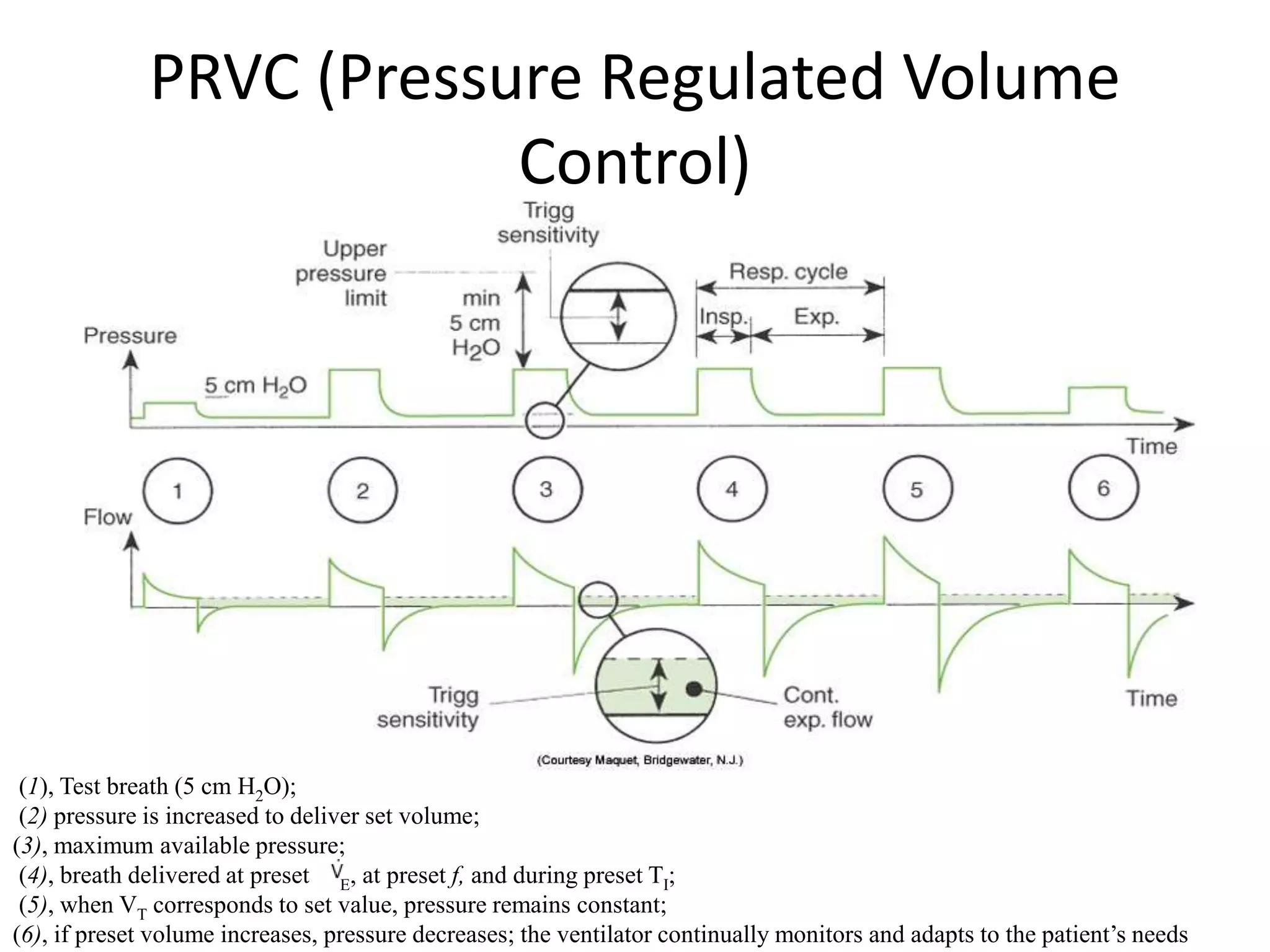
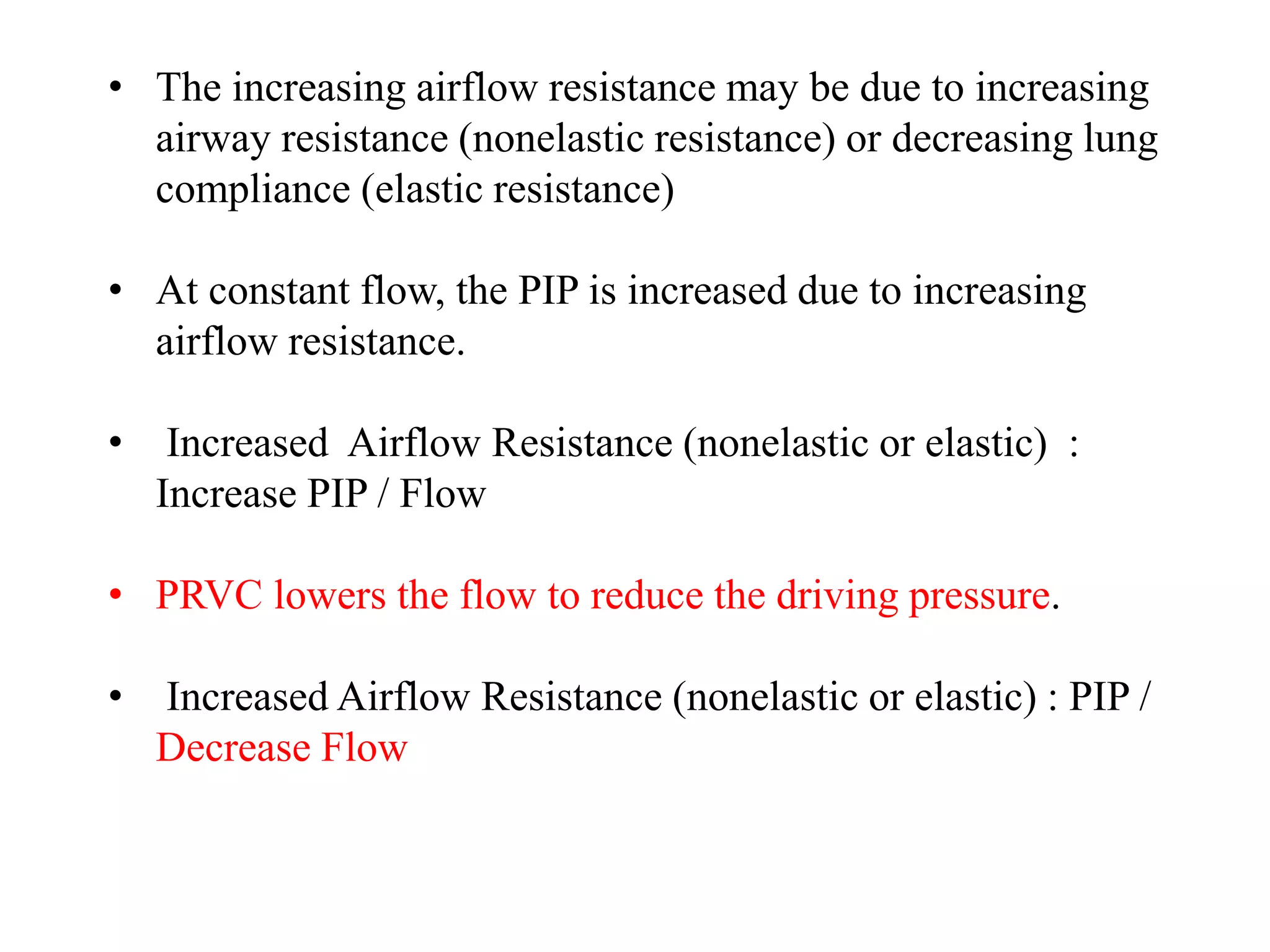
The document discusses several newer modes of mechanical ventilation including volume assured pressure support (VAPS), volume support (VS), pressure regulated volume control (PRVC), and adaptive support ventilation (ASV). VAPS switches between pressure control and volume control modes within a breath to ensure a minimum tidal volume. VS adjusts pressure support levels between breaths to maintain a target tidal volume. PRVC aims to deliver a set tidal volume with the lowest possible airway pressure by modifying flow and time. ASV automatically adapts support levels to provide a minimum minute ventilation with the least work of breathing.