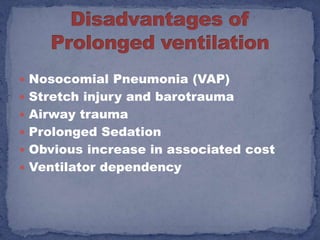
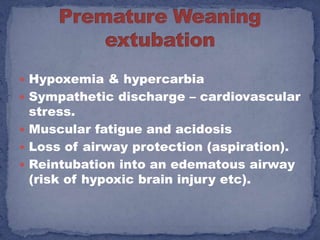
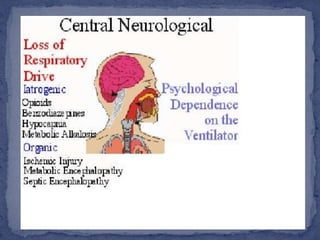
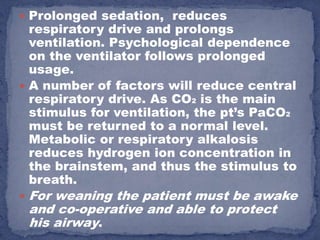
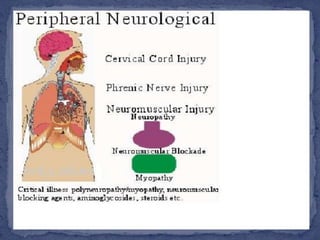
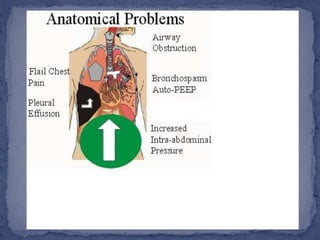
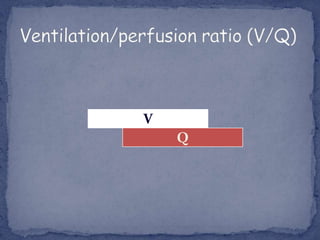
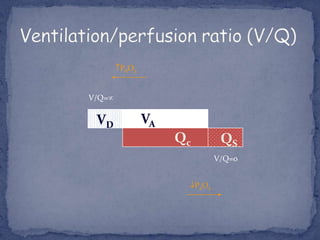
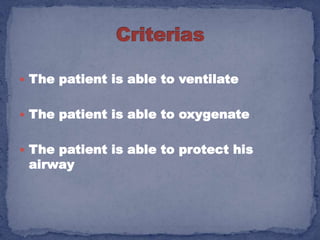
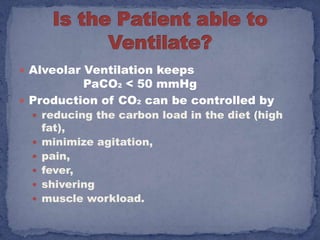
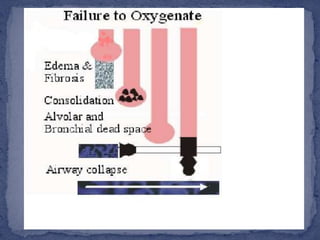
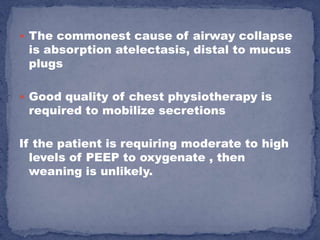
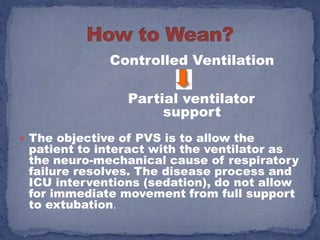
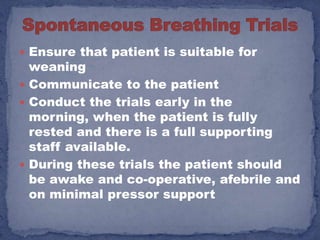
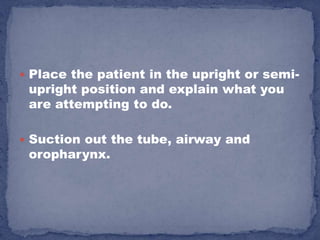
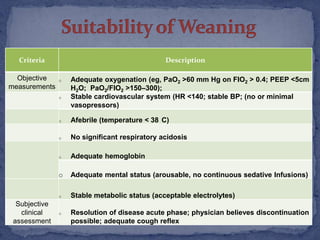
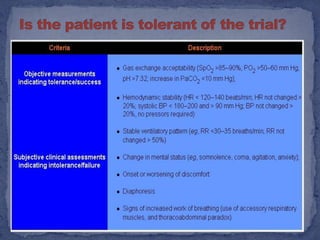
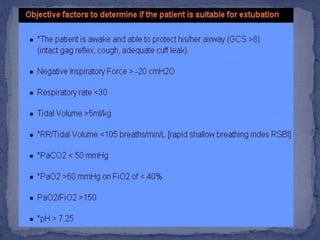
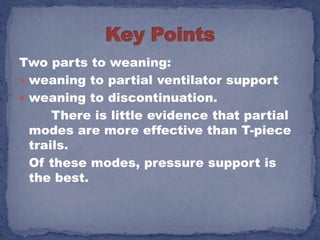
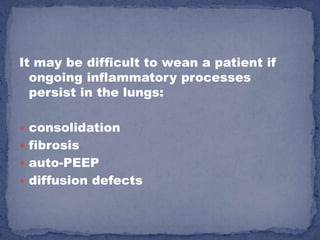
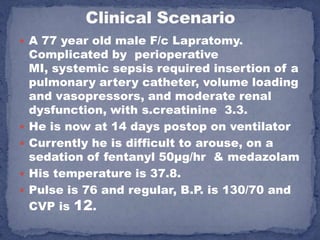
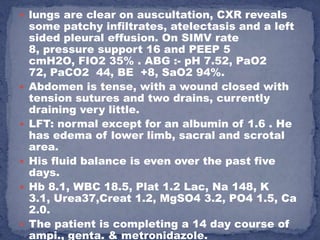
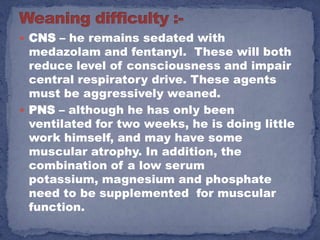
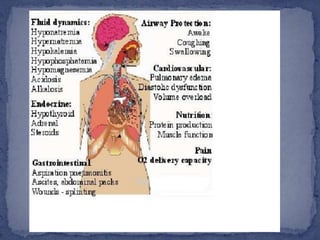
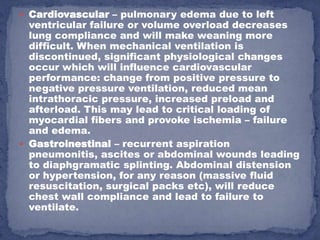
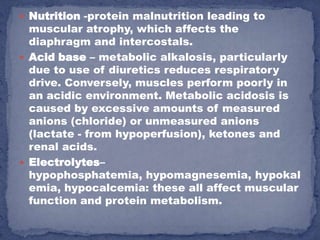
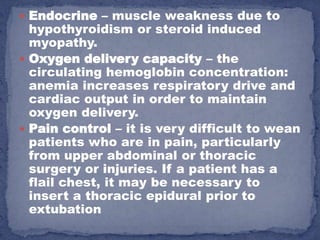
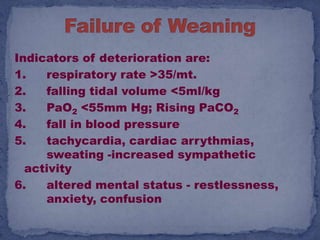
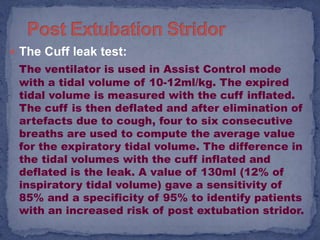
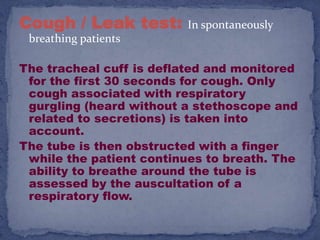
This document discusses factors to consider when removing a patient from mechanical ventilation (weaning). It outlines criteria to assess patient readiness, including respiratory function, oxygenation, hemodynamics, neurological status, secretions and comorbidities. Complications of failed weaning are also described. Key considerations involve addressing sedation, electrolyte imbalances, infection/inflammation and optimizing cardiac, nutritional and acid-base status.