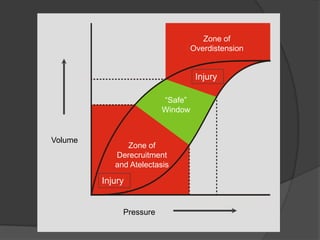
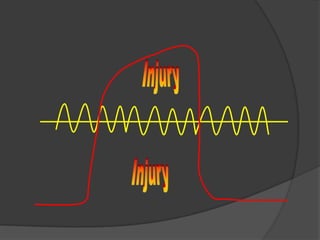
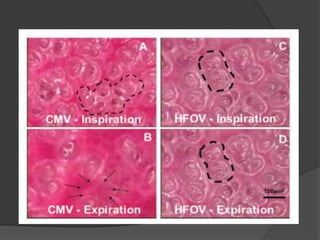
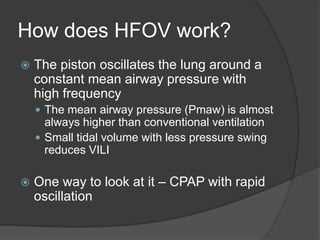
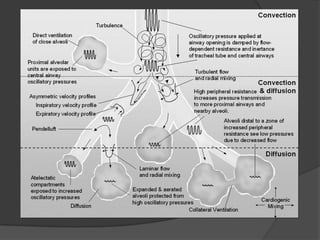
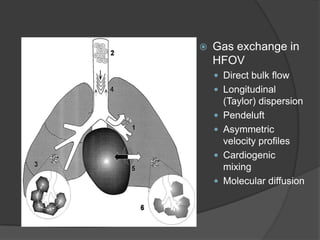
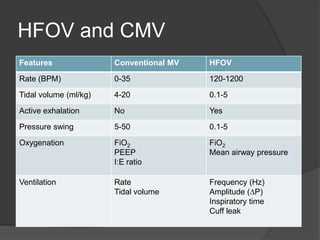
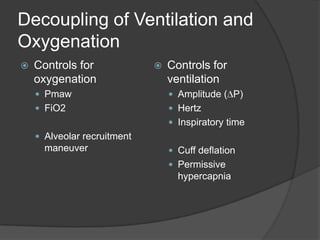
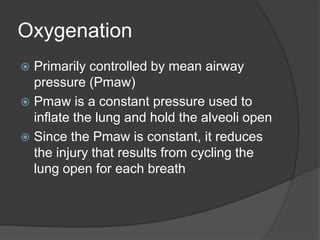
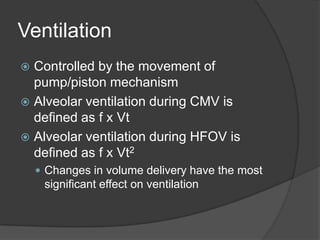
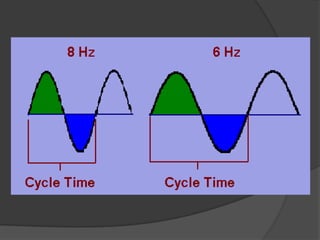
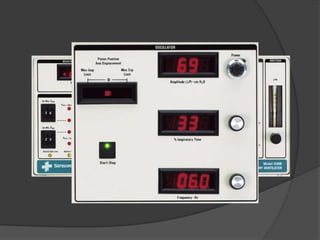
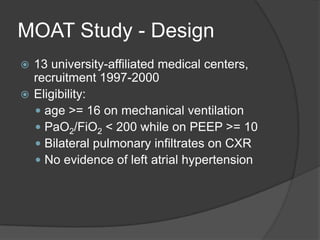
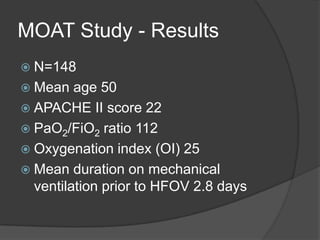
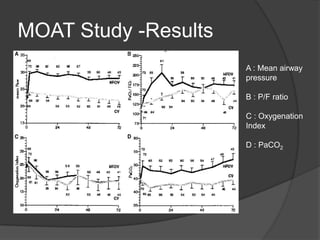
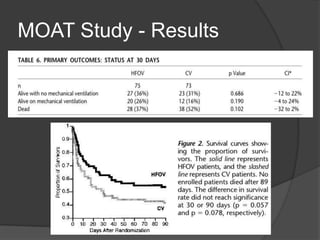
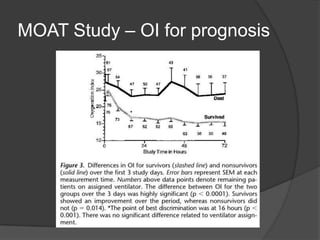
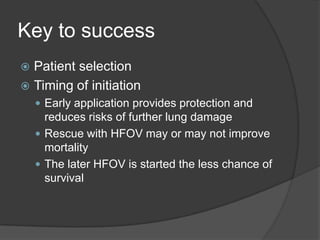
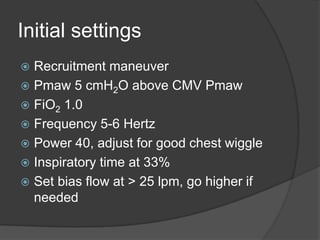
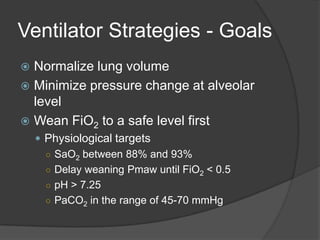
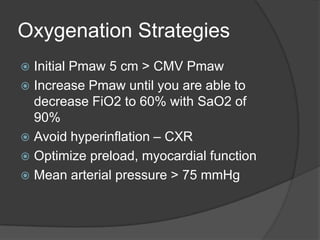
HFOV uses small, rapid lung oscillations to reduce ventilator-induced lung injury compared to conventional mechanical ventilation. It works by maintaining constant mean airway pressure and small tidal volumes to avoid alveolar overdistension and collapse. Several early studies found HFOV improved oxygenation compared to CMV for ARDS, but larger trials found no significant difference in mortality. Proper patient selection, early initiation, and careful titration of pressures and settings are key to optimize outcomes with HFOV.