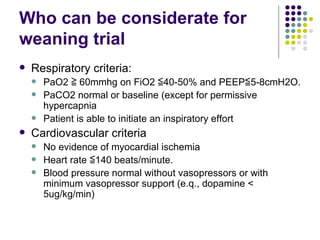
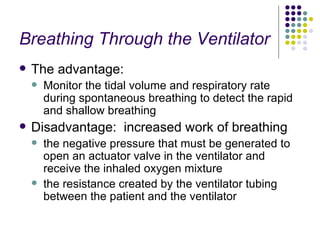
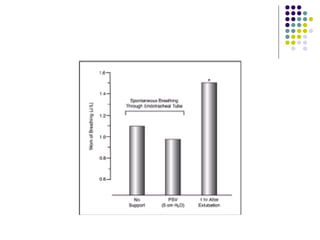
The document discusses criteria for determining when a patient can be safely removed from mechanical ventilation, including assessments of respiratory, cardiovascular and mental status. It describes methods used to identify patients who can tolerate a spontaneous breathing trial, such as the rapid shallow breathing index. The document also outlines protocols for conducting spontaneous breathing trials through a ventilator or T-piece and managing issues that could arise like respiratory failure, low cardiac output, or laryngeal edema.