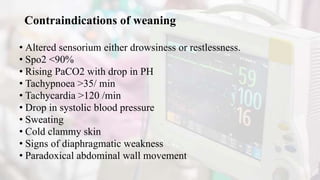
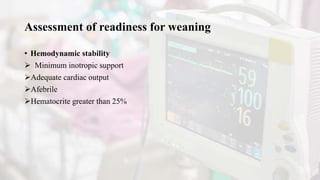
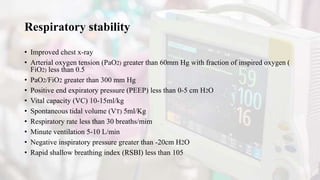
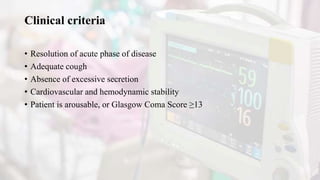
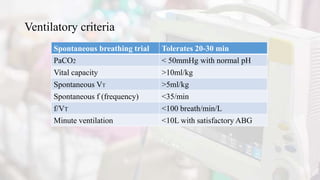
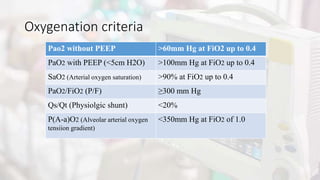
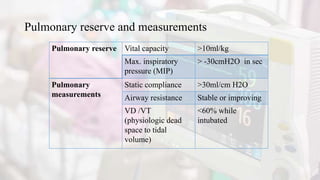
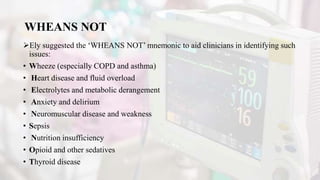
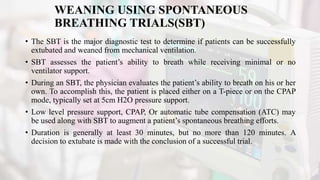
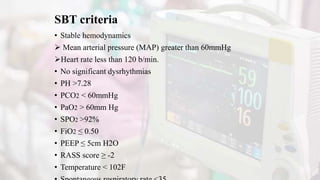
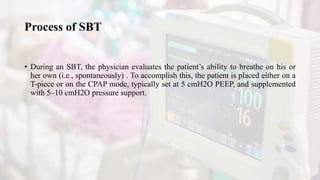
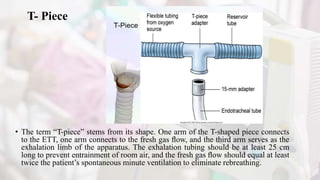
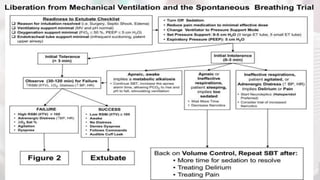
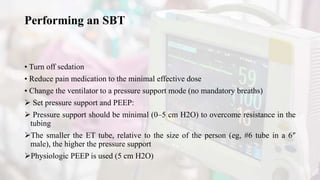
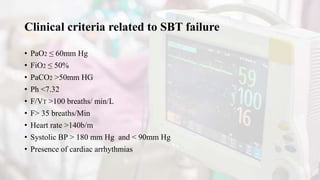
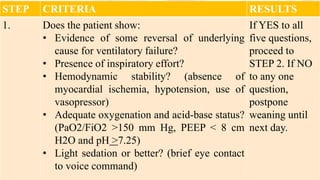
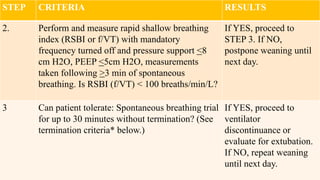
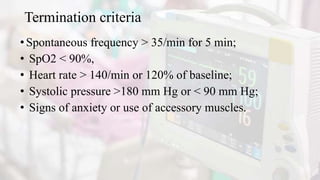
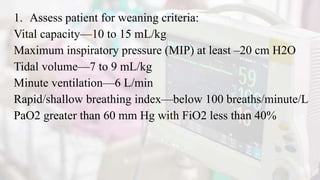
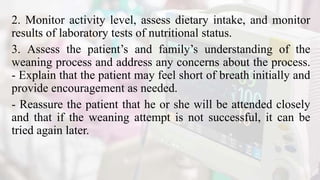
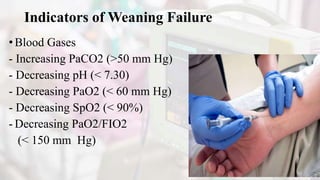
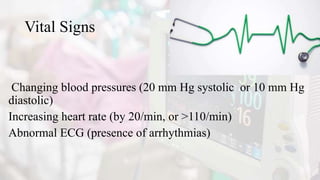
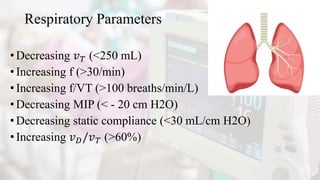
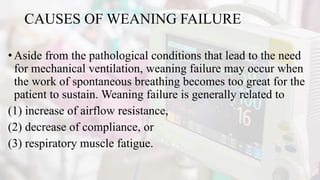
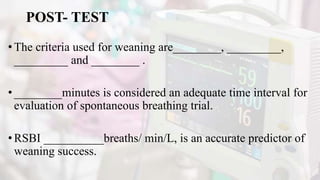
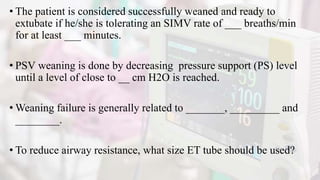
The document discusses the process of weaning patients from mechanical ventilation, emphasizing the assessment of readiness, criteria for weaning, and the various methods involved, such as spontaneous breathing trials (SBT) and progressive withdrawal of mechanical support. It outlines important indicators, contraindications, and factors contributing to difficult weaning, and establishes the criteria necessary for successfully transitioning patients off mechanical ventilators. The document also highlights the significance of monitoring patient response during weaning trials to ensure safety and effectiveness.