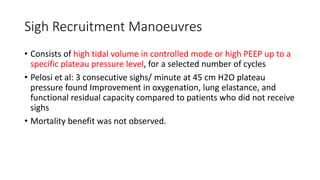
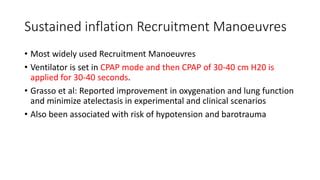
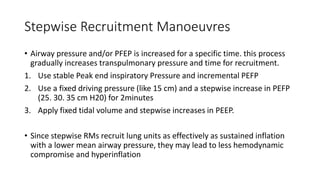
1) Recruitment maneuvers (RMs) aim to reopen collapsed alveoli in ARDS patients through temporarily increasing transpulmonary pressure. Common types include sighs, sustained inflations, and stepwise increases in pressure.
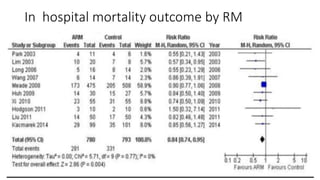
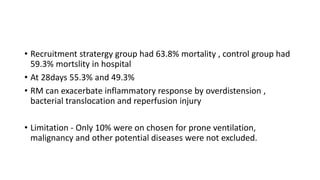
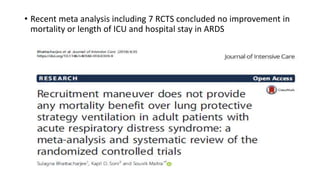
2) While RMs often improve short-term oxygenation, clinical trials have found no evidence of reduced mortality or improved outcomes. One large trial found RMs may actually increase mortality.
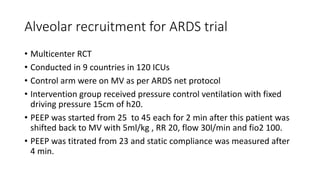
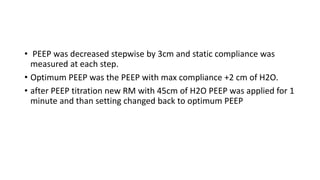
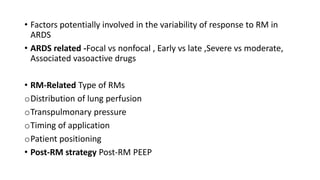
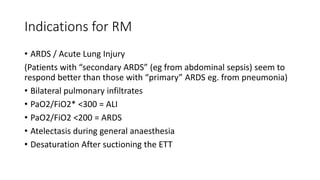
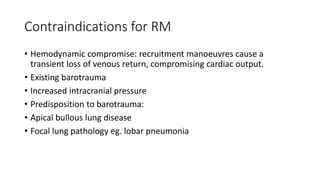
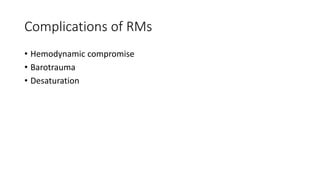
3) Not all ARDS patients respond equally to RMs due to factors like etiology, severity, and lung recruitability. RMs should only be considered for hypoxemic individuals based on an individual risk-benefit assessment.