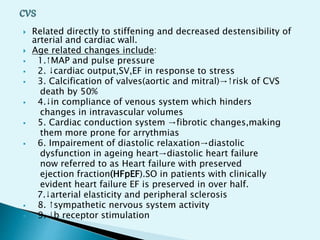
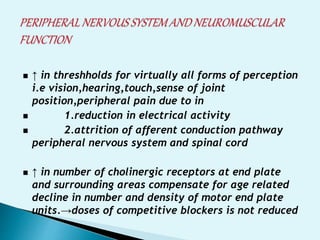
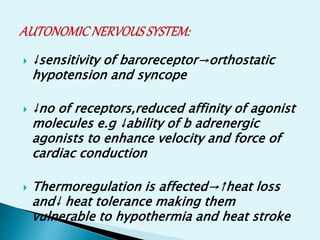
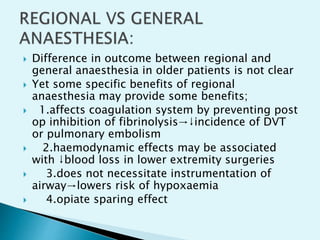
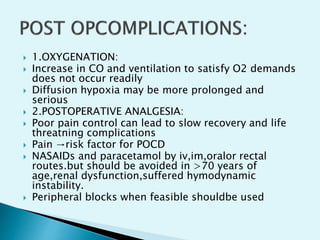
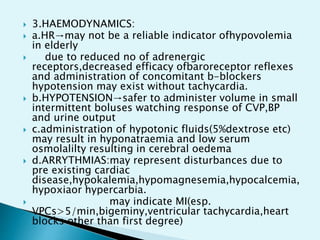
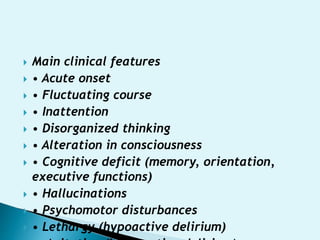
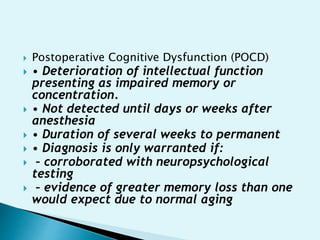
Elderly patients represent the fastest growing population globally. They experience many age-related physiological changes that increase surgical risk. Preoperative evaluation and optimization is important to identify risks like cardiovascular disease and pulmonary issues. Anesthesia in the elderly requires lower doses of induction agents and opioids due to pharmacokinetic changes. Regional anesthesia may provide benefits over general anesthesia. Close postoperative monitoring is needed due to risks of complications like delirium, cognitive dysfunction, hypotension, and hypothermia.