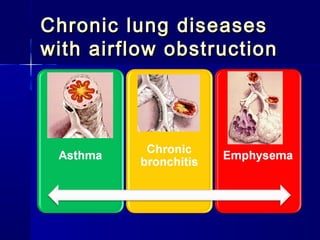
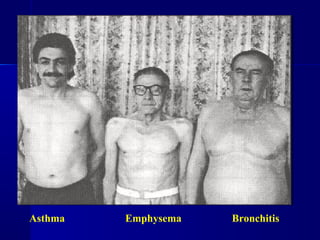
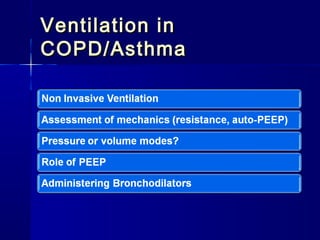
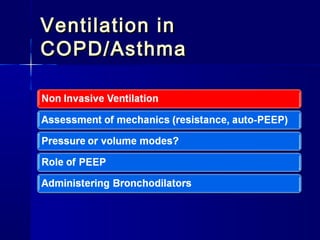
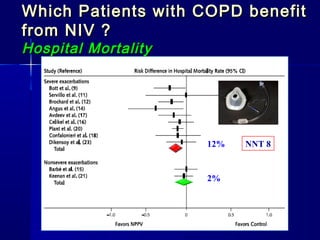
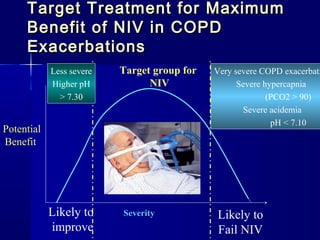
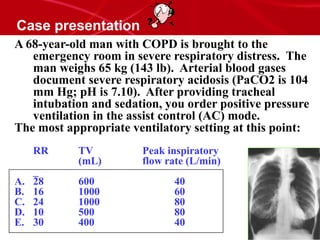
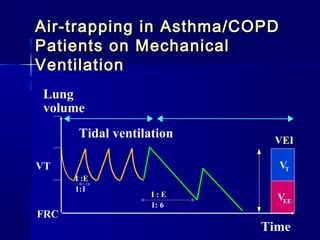
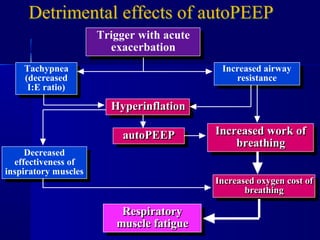
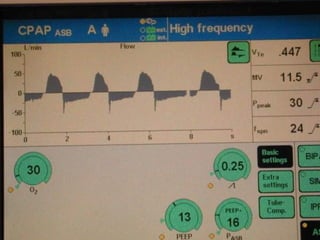
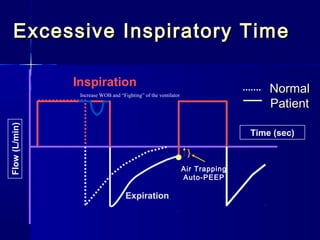
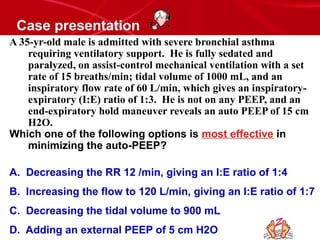
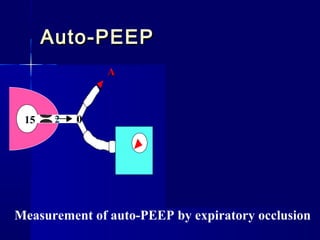
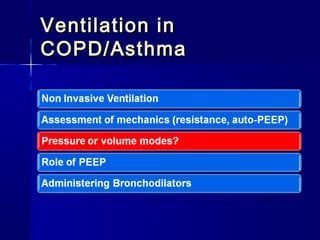
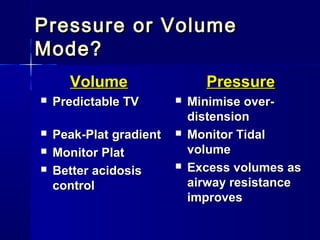
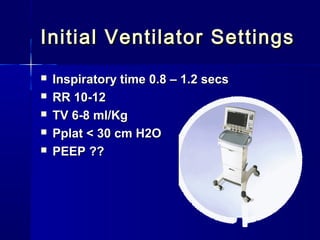
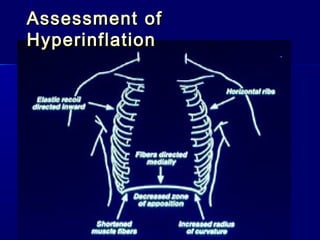
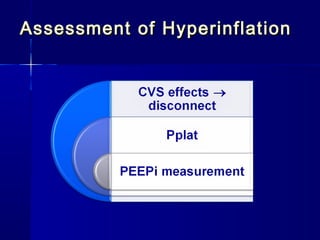
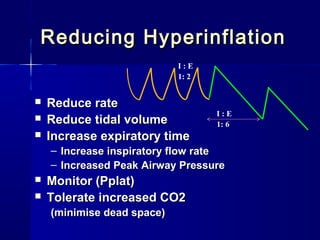
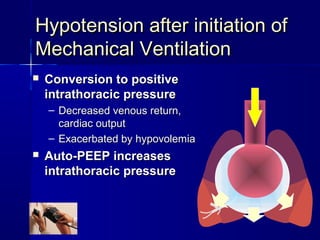
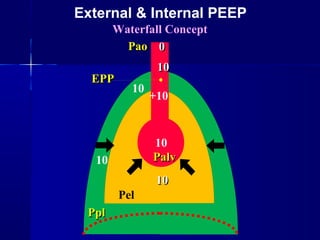
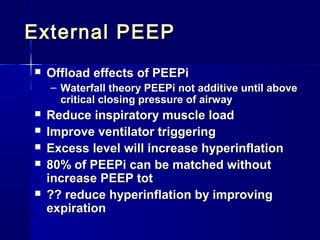
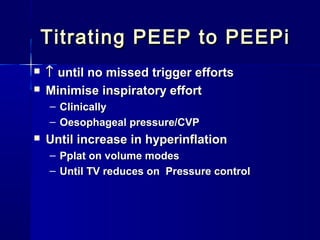
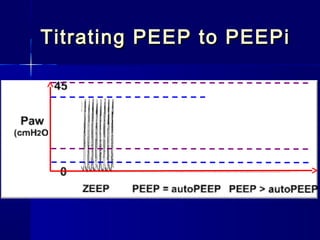
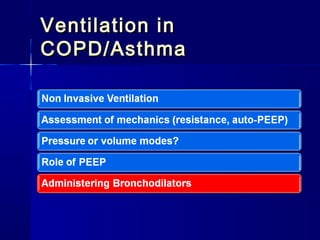
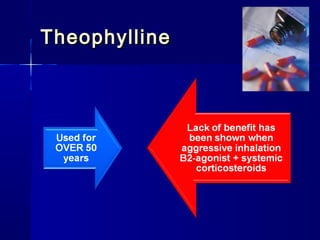
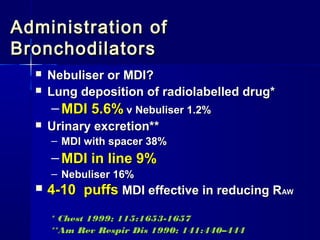
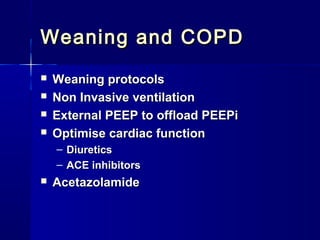
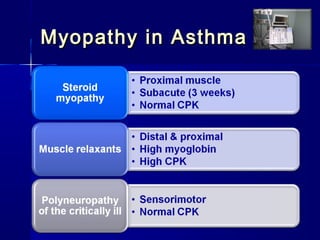
This document discusses mechanical ventilation for patients with severe chronic lung diseases causing airflow obstruction such as COPD and asthma. It provides guidance on appropriate ventilator settings and strategies to minimize issues like auto-PEEP and hyperinflation. These include adjusting respiratory rate, tidal volume, inspiratory time and adding external PEEP. Proper use of bronchodilators via nebulizer or metered dose inhaler is also reviewed. Weaning from ventilation can be challenging in COPD but protocols and non-invasive ventilation can help. Optimizing cardiac function and treating complications like myopathy are also important.