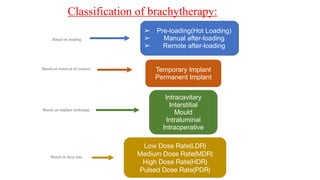
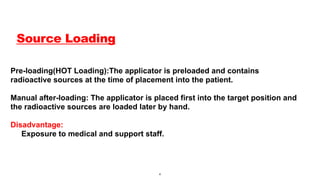
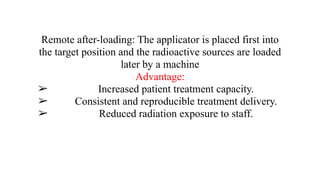
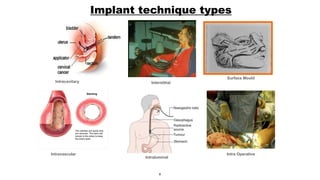
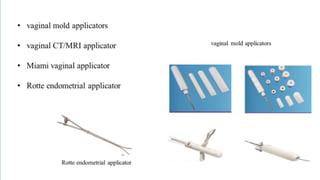
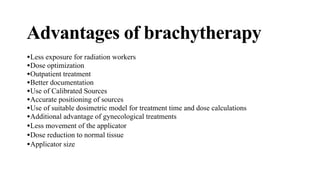
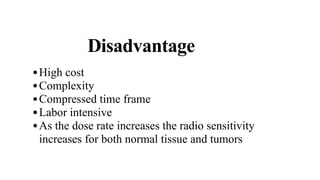
Brachytherapy is a cancer treatment method that uses sealed radioactive sources placed inside or near a tumor to deliver radiation. It can be classified based on loading methods, implant techniques, and dose rates, with various applicators developed for precise dose delivery. While it offers advantages like outpatient treatment and reduced radiation exposure for staff, it also has disadvantages such as high costs and complexity.