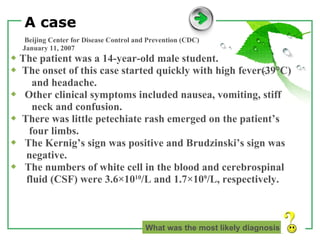
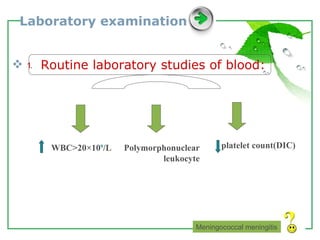
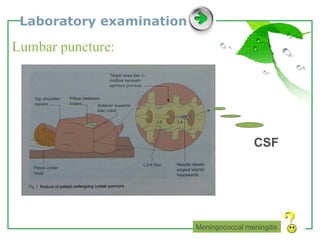
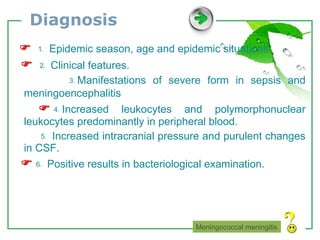
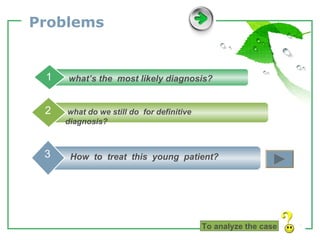
1. The document describes a case of meningococcal meningitis in a 14-year-old male student who presented with high fever, headache, nausea, vomiting, stiff neck and confusion. Examination found a positive Kernig's sign and white blood cell counts were elevated in both blood and cerebrospinal fluid.
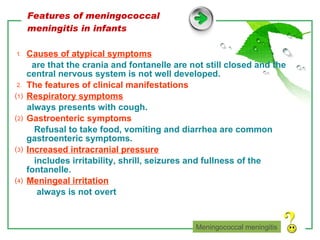
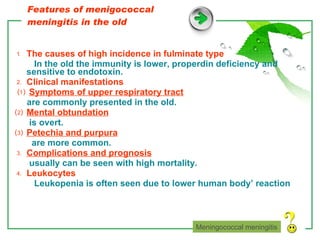
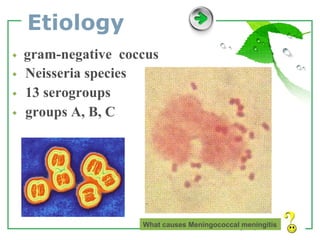
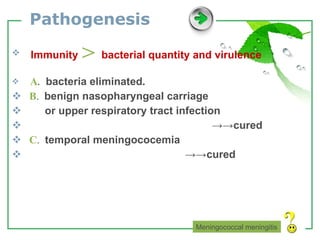
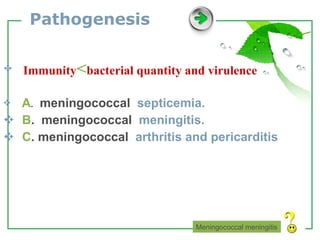
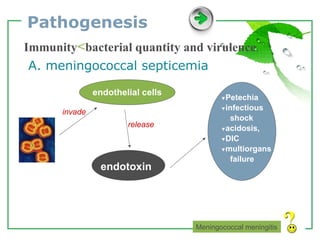
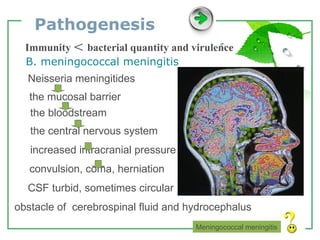
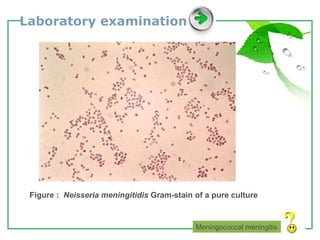
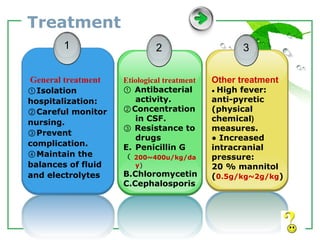
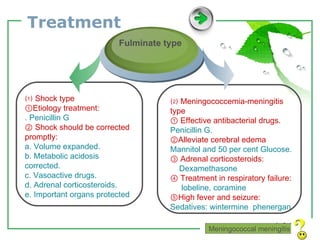
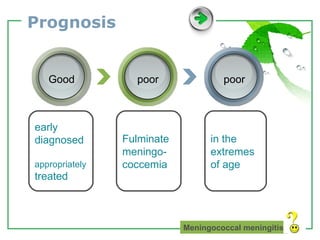
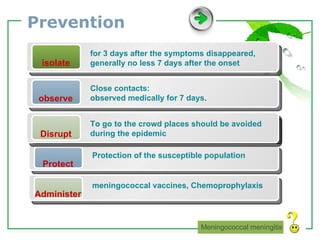
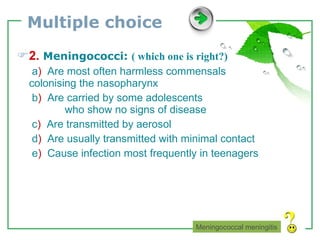
2. The document then provides background information on meningococcal meningitis, including that it is caused by Neisseria meningitidis bacteria, signs and symptoms, routes of transmission, risk groups, treatment which includes antibiotics and supportive care, and prevention through vaccination and chemoprophylaxis of close contacts.
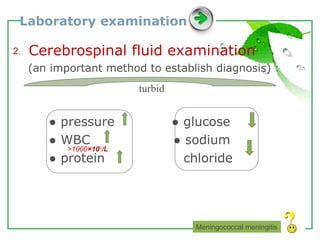
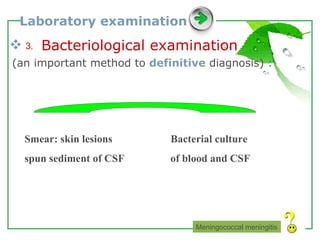
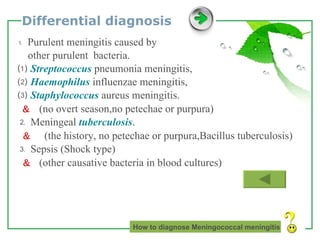
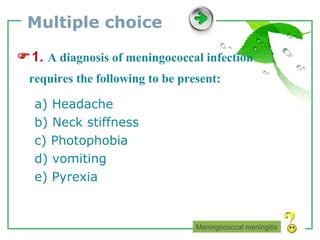
3. Differential diagnoses and diagnostic testing are also






![Thank You for your suggestion! E-mail: [email_address] Qq: 673162735](https://image.slidesharecdn.com/4-meningococcalmeningitis-100319060104-phpapp01/85/4-Meningococcal-Meningitis-36-320.jpg)