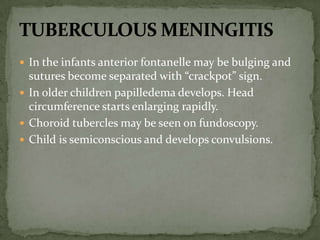
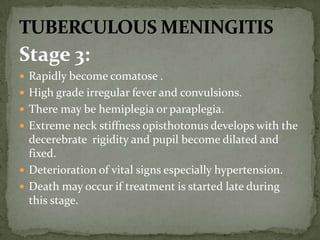
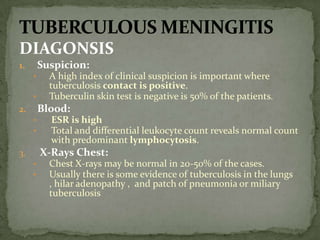
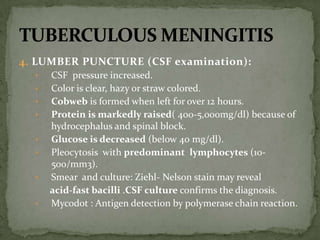
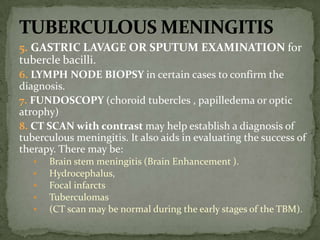
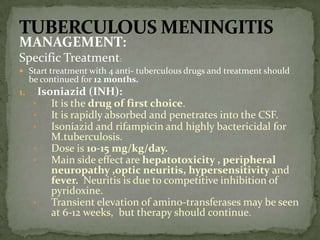
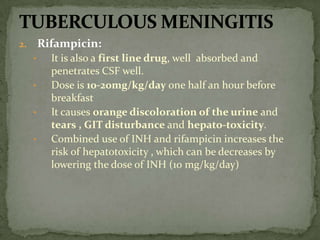
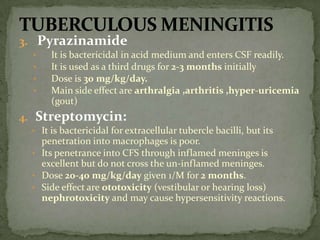
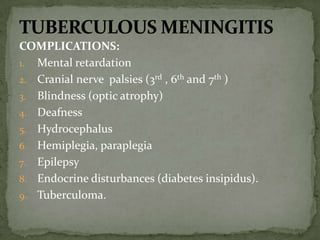
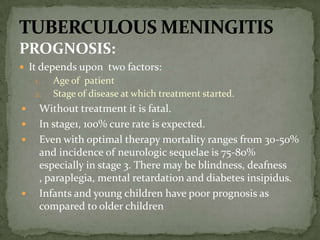
Tuberculous meningitis is inflammation of the membranes surrounding the brain and spinal cord caused by Mycobacterium tuberculosis. It typically develops secondary to a pulmonary tuberculosis infection. Symptoms progress through three stages - an initial prodromal stage with nonspecific symptoms, followed by signs of meningeal irritation and cranial nerve palsies, and finally a terminal stage with coma and death if untreated. Diagnosis involves lumbar puncture showing lymphocytic pleocytosis and decreased glucose. Treatment consists of a combination of antitubercular drugs for 12 months along with corticosteroids to reduce inflammation and complications. Prognosis depends on the stage of disease at treatment initiation, with mortality rates as high as 50%