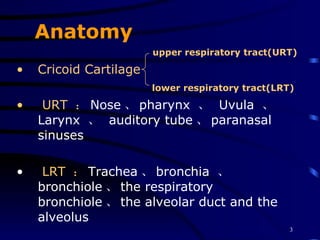
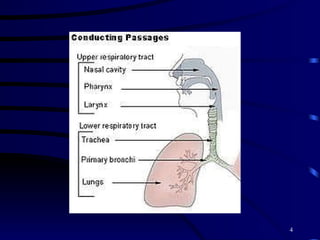
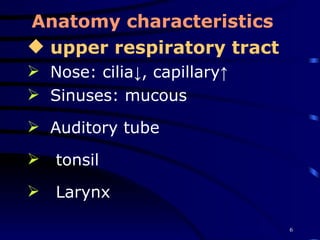
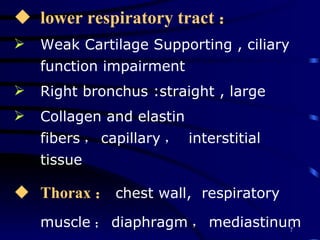
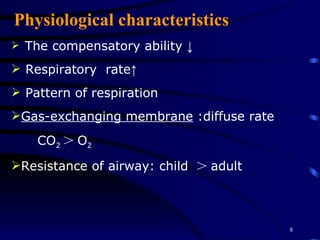
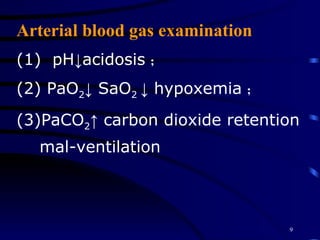
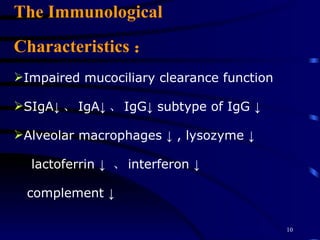
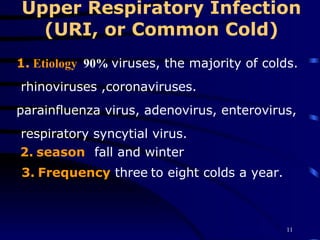
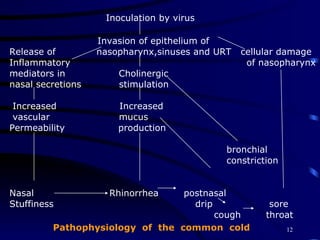
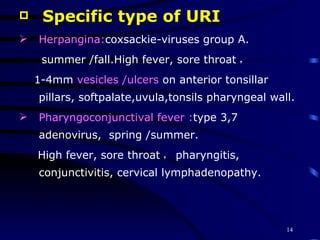
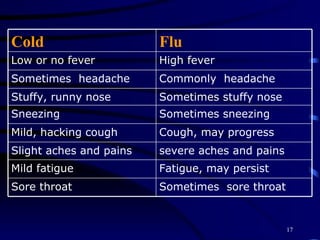
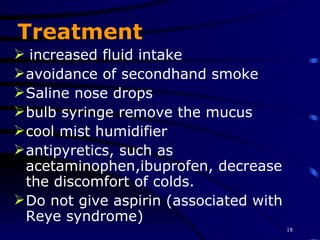
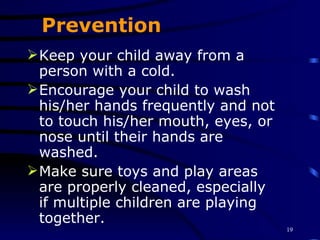
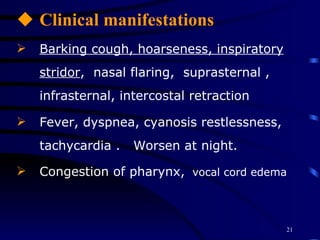
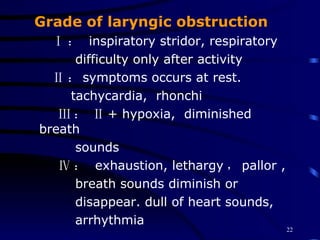
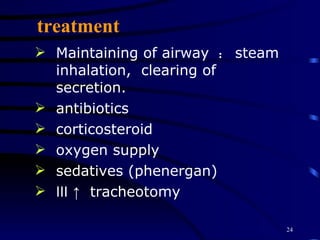
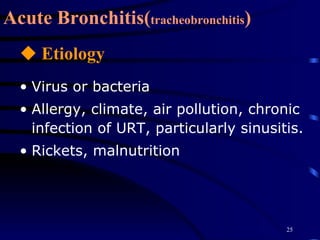
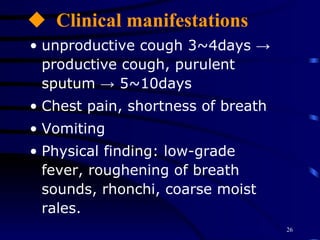
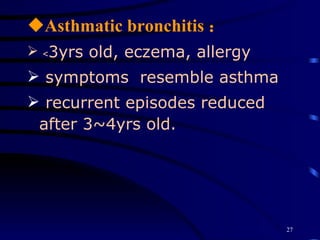
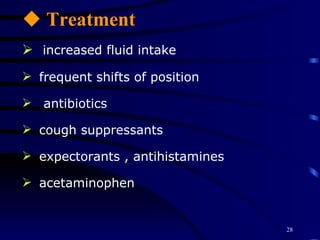
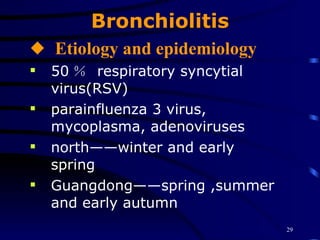
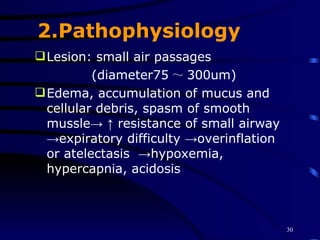
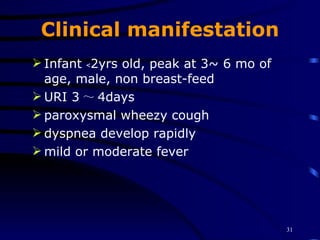
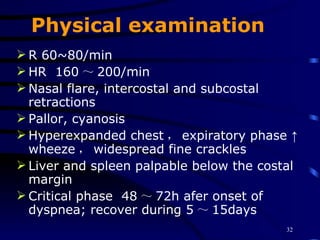
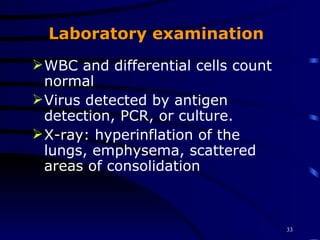
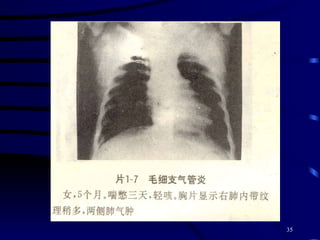
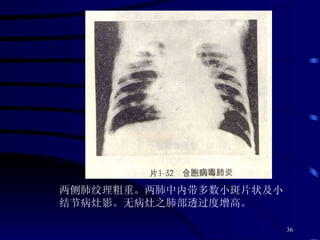
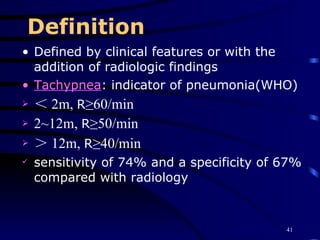
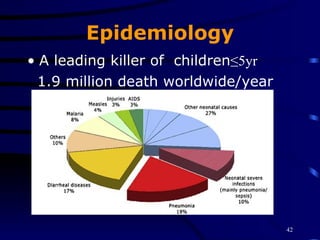
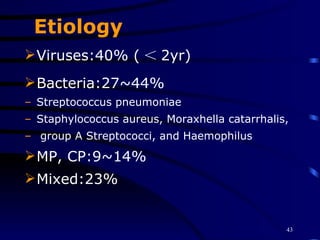
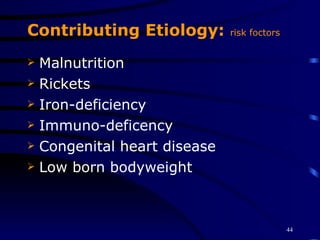
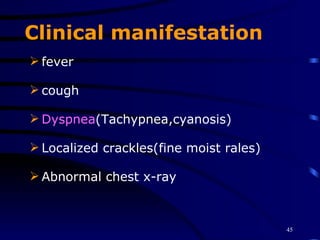
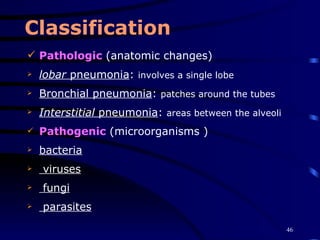
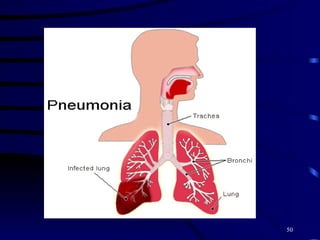
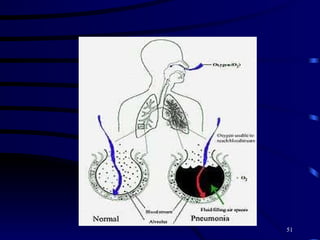
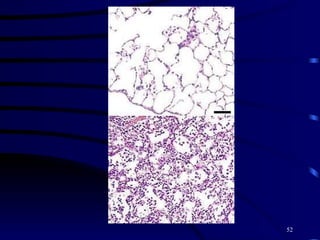
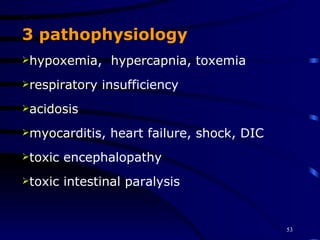
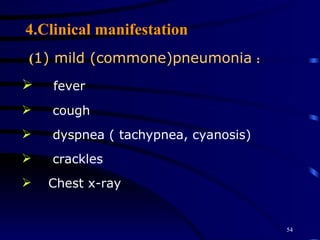
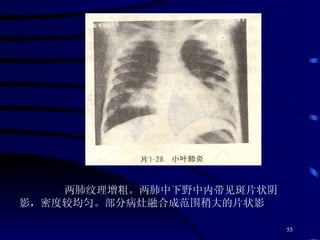
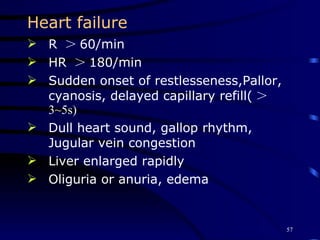
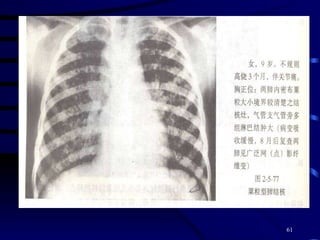
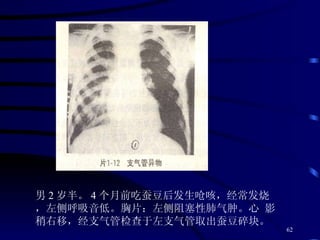
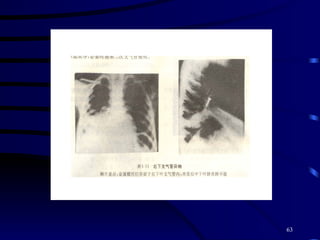
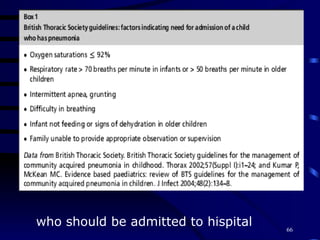
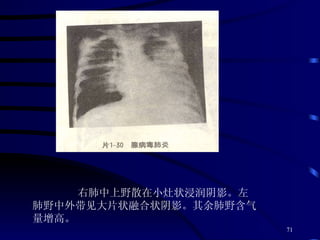
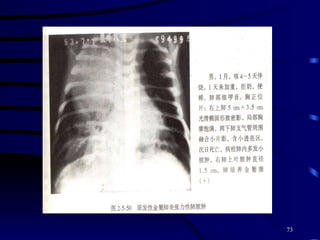
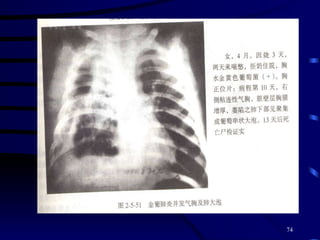
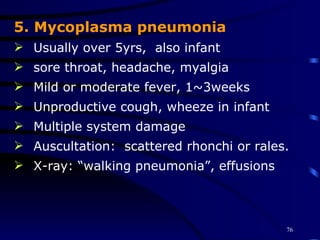
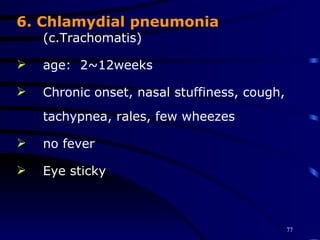
The document summarizes various respiratory tract infections, including their etiology, clinical manifestations, treatment and prevention. It discusses upper respiratory infections like the common cold, acute infectious laryngitis and acute bronchitis. It also covers lower respiratory infections such as bronchiolitis, pneumonia caused by different pathogens like RSV, adenovirus and Staphylococcus aureus. Diagnosis, classifications, complications and management of pneumonia are described.