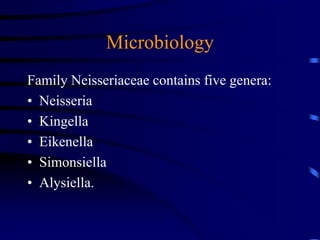
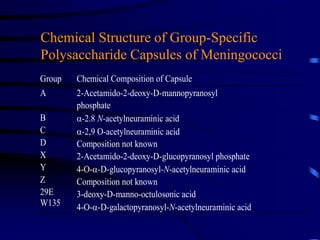
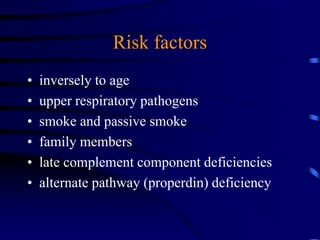
Meningococcal disease is a severe bacterial infection that causes rapid onset of fever, headache, and a rash. It can progress quickly and cause death within hours if not treated. The disease is caused by Neisseria meningitidis bacteria, which are spread through respiratory and throat secretions. Serogroups A, B, and C account for most cases worldwide. Symptoms include sudden high fever, headache, stiff neck, confusion, and a red-purple rash. Diagnosis is made through cultures, gram stains, and PCR testing of spinal fluid or blood. Treatment involves intravenous antibiotics like penicillin or ceftriaxone. Contacts are given antibiotic prophylaxis and vaccination to prevent further