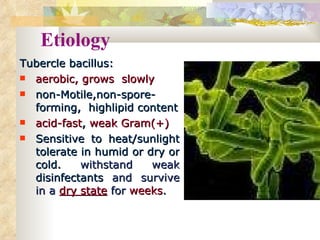
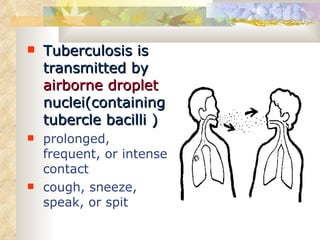
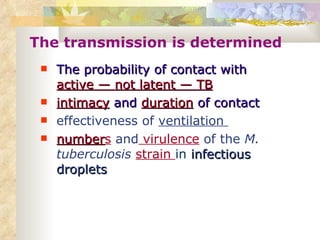
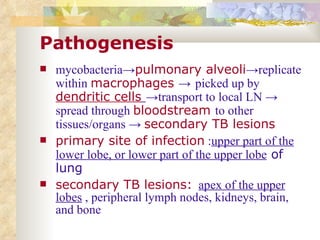
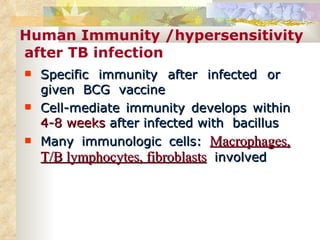
- Tuberculosis is caused by the bacterium Mycobacterium tuberculosis and mainly affects the lungs, but can spread to other organs. It is transmitted through airborne droplets when infected people cough, sneeze or speak.
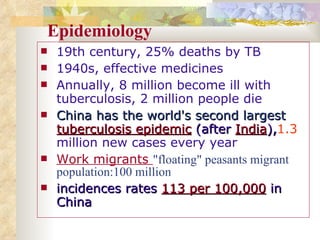
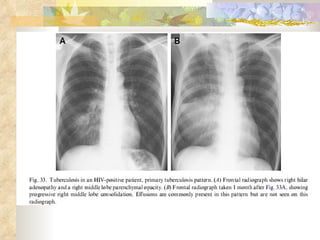
- China has the second largest tuberculosis epidemic in the world after India, with over 1.3 million new cases reported each year. Risk factors include poverty, malnutrition, HIV infection, and living/working conditions like overcrowding.
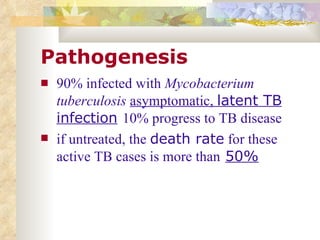
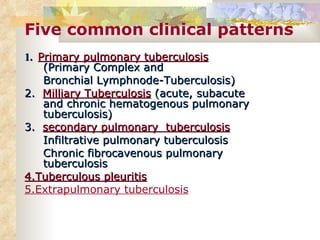
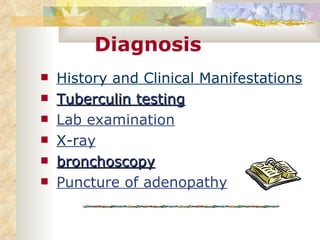
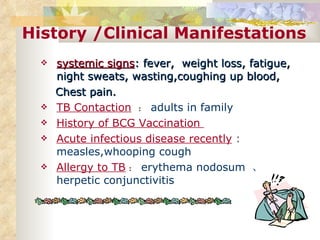
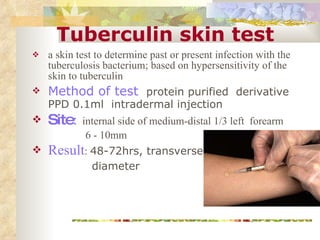
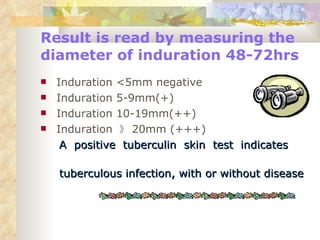
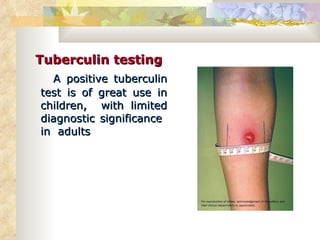
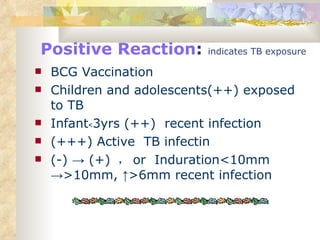
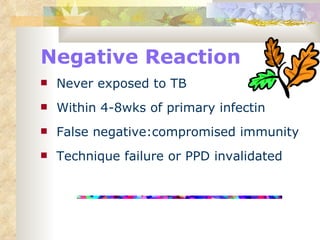
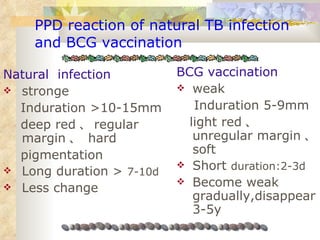
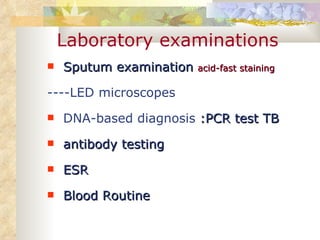
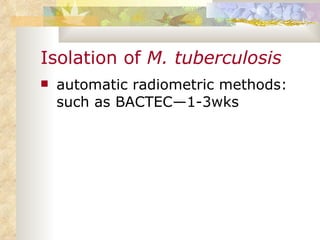
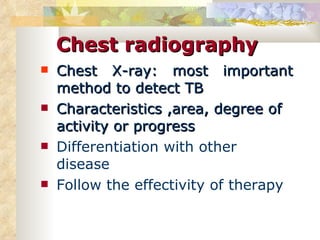
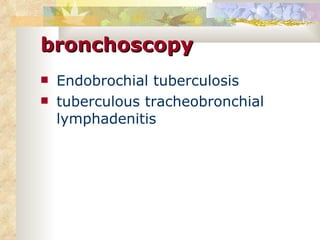
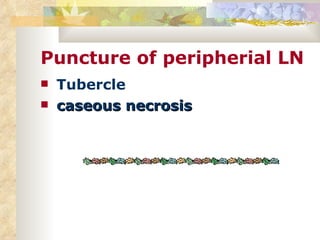
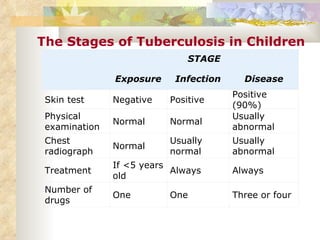
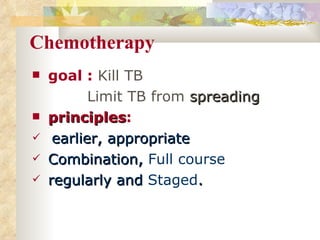
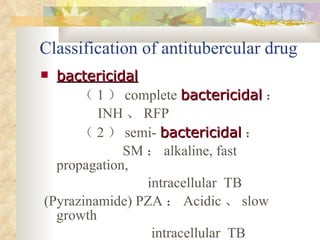
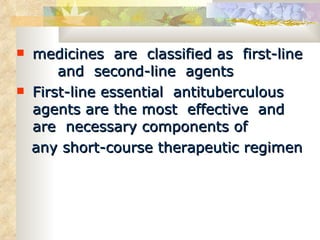
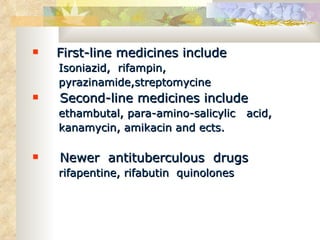
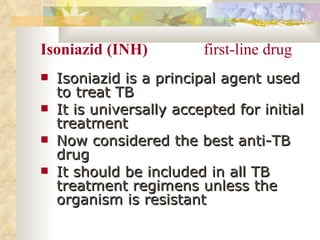
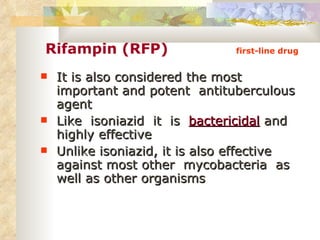
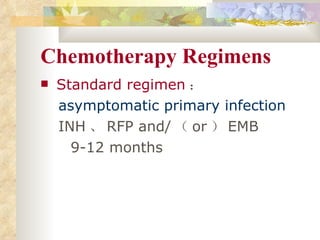
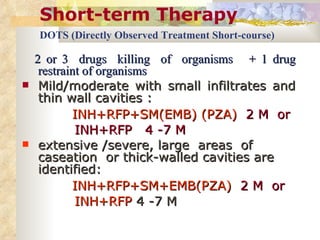
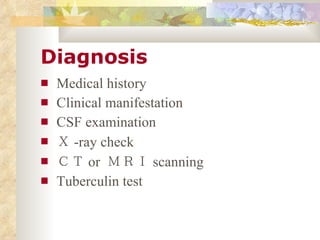
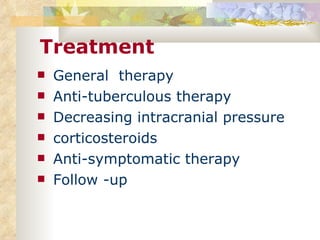
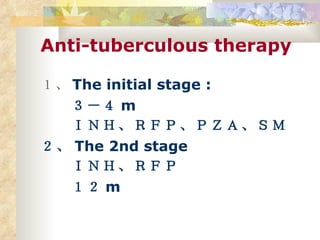
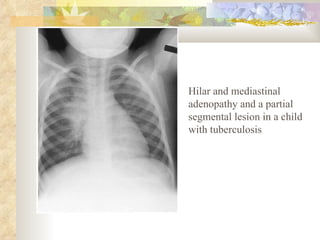
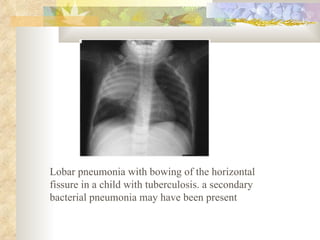
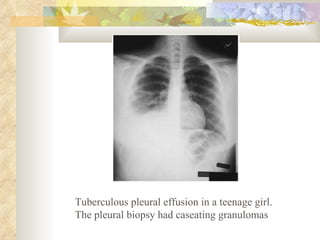
- Tuberculosis infection can either remain latent or progress to active disease. Diagnosis involves tuberculin skin tests, chest x-rays, sputum smears, and culture tests. Standard treatment uses a combination of antibiotics like isoniazid and