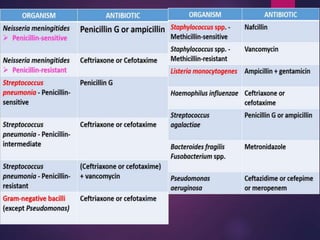
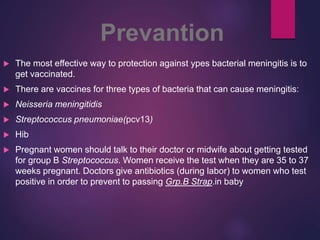
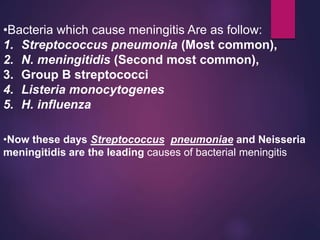
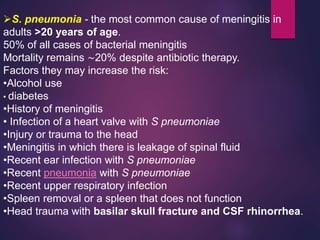
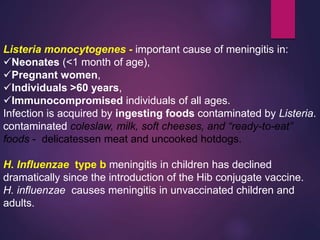
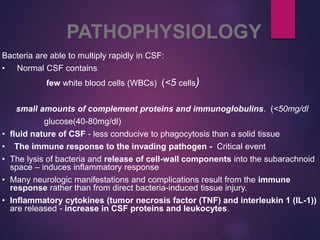
Bacterial meningitis is a serious infection of the membranes surrounding the brain and spinal cord. It is usually caused by bacteria such as Streptococcus pneumoniae or Neisseria meningitidis. Symptoms include sudden onset of fever, headache, and neck stiffness. Without prompt treatment, bacterial meningitis can cause death or permanent disability. Diagnosis involves examination of cerebrospinal fluid obtained through lumbar puncture. Empirical antibiotic therapy with drugs such as ceftriaxone and vancomycin is started immediately while diagnostic tests are pending. Vaccination is the most effective way to prevent certain types of bacterial meningitis.



![Diagnosis
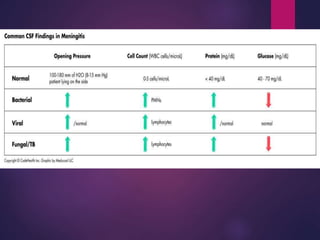
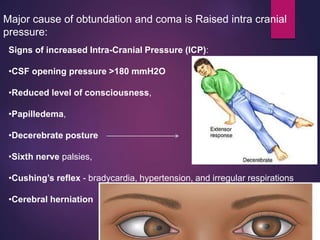
• The classic CSF abnormalities in bacterial meningitis are:
1. polymorphonuclear (PMN) leukocytosis (>100 cells/μL in
90%),
2. Decreased glucose concentration [<2.2 mmol/L (<40
mg/dL)
3. CSF/ serum glucose ratio of <0.4 in ∼60%,
4. Increased protein concentration [>0.45 g/L (>45 mg/dL) in
90%],
5. Increased opening pressure (>180 mmH2O in 90%).
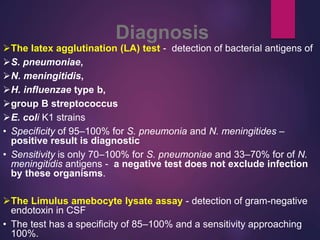
6. CSF bacterial cultures - positive in >80% of patients,
7. CSF Gram’s stain demonstrates organisms in >60%
• PCR - detect small numbers of organisms in CSF – used in
patients who have been pretreated with antibiotics
• If LP is delayed to obtain neuroimaging studies - empirical](https://image.slidesharecdn.com/infectiouspresention12-180304230212/85/bacterial-meningitis-15-320.jpg)