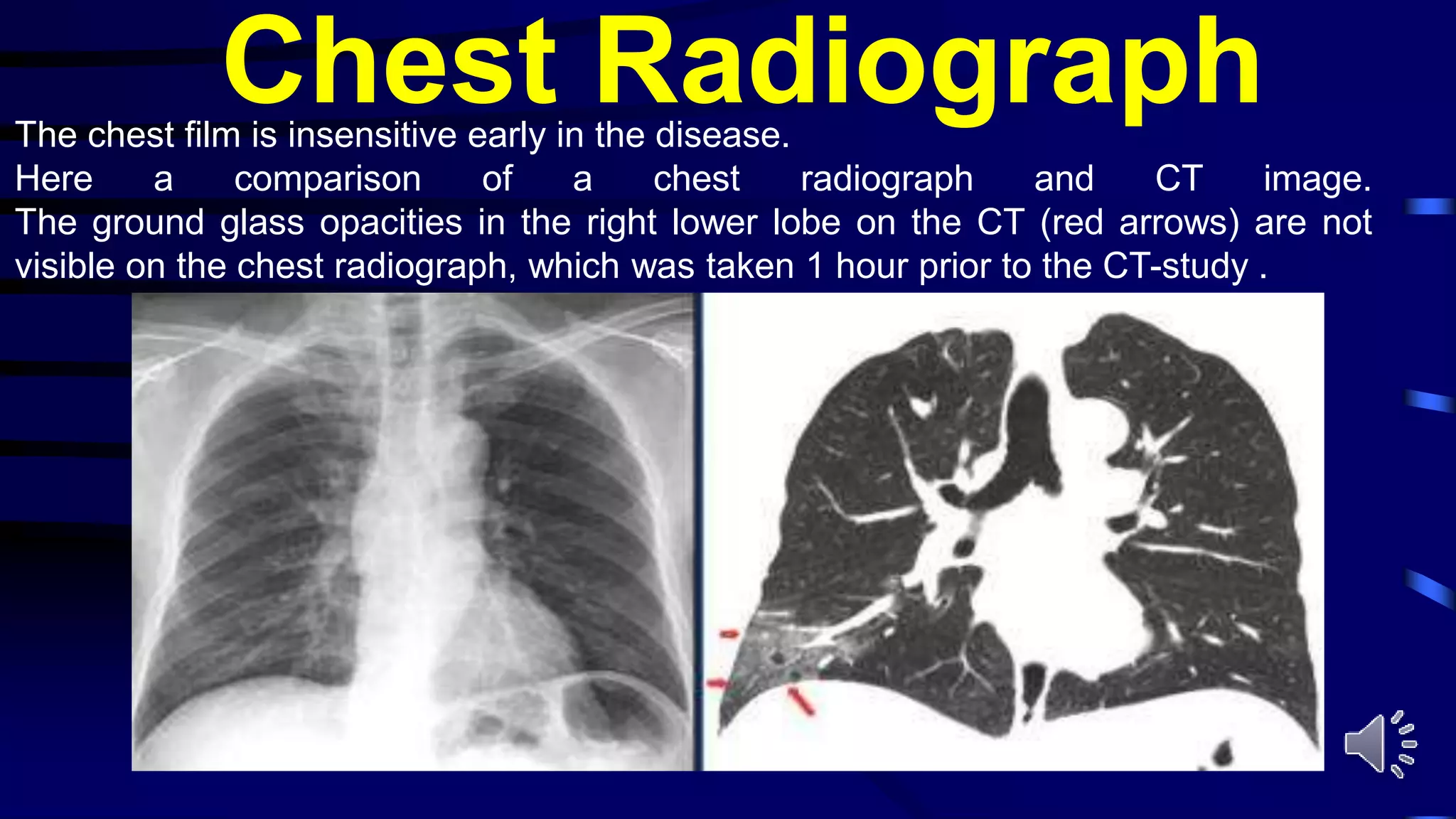
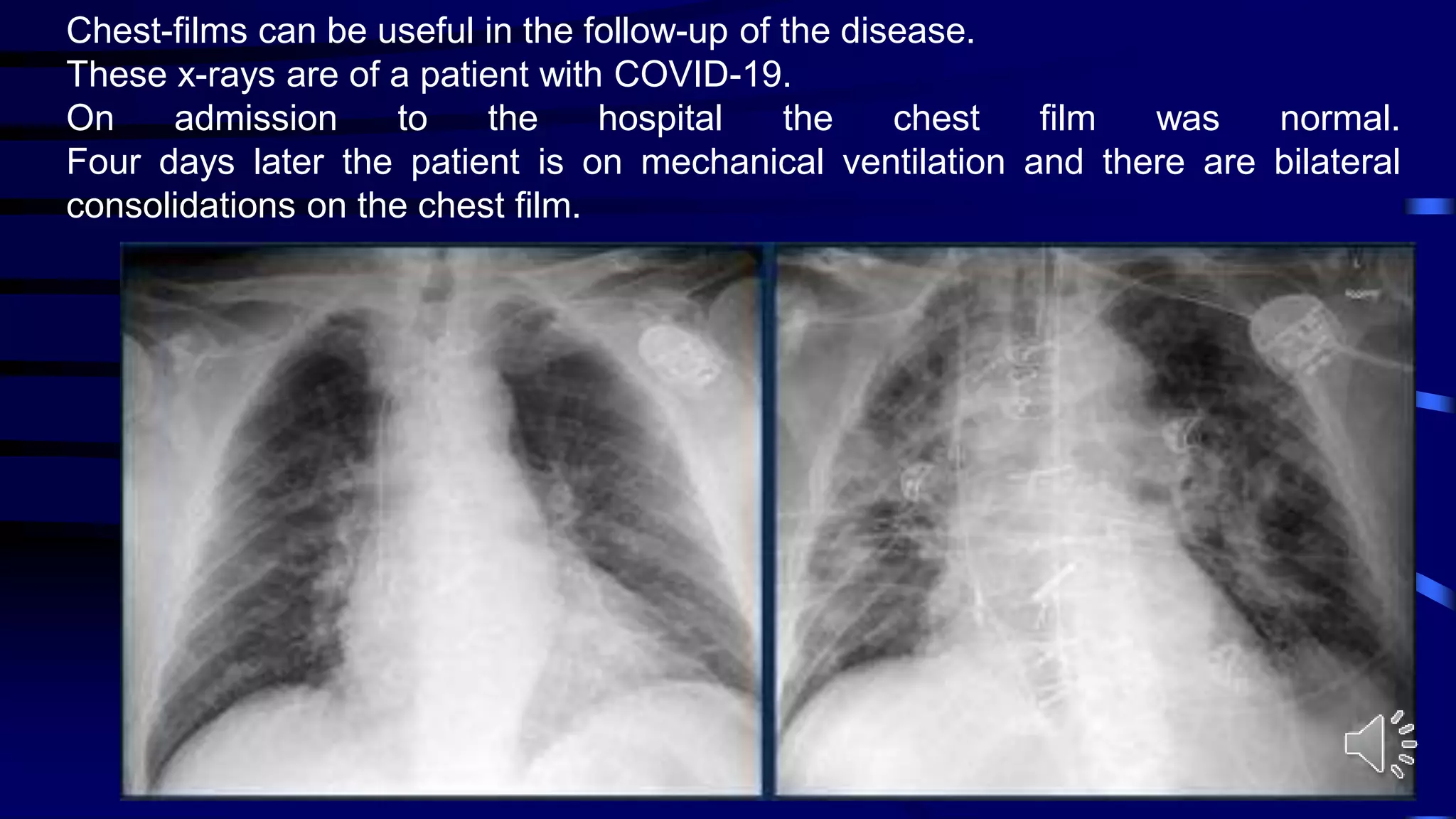
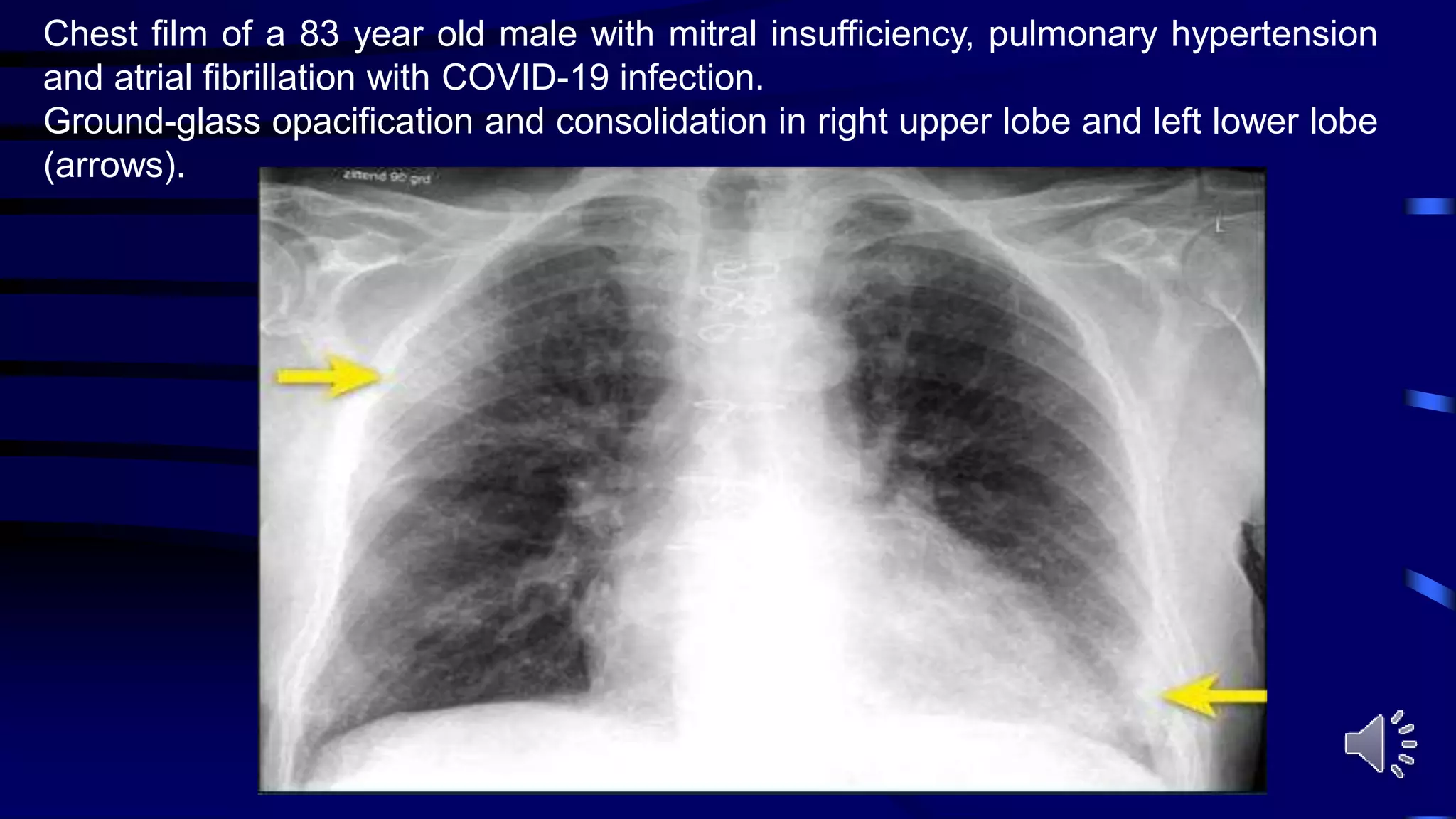
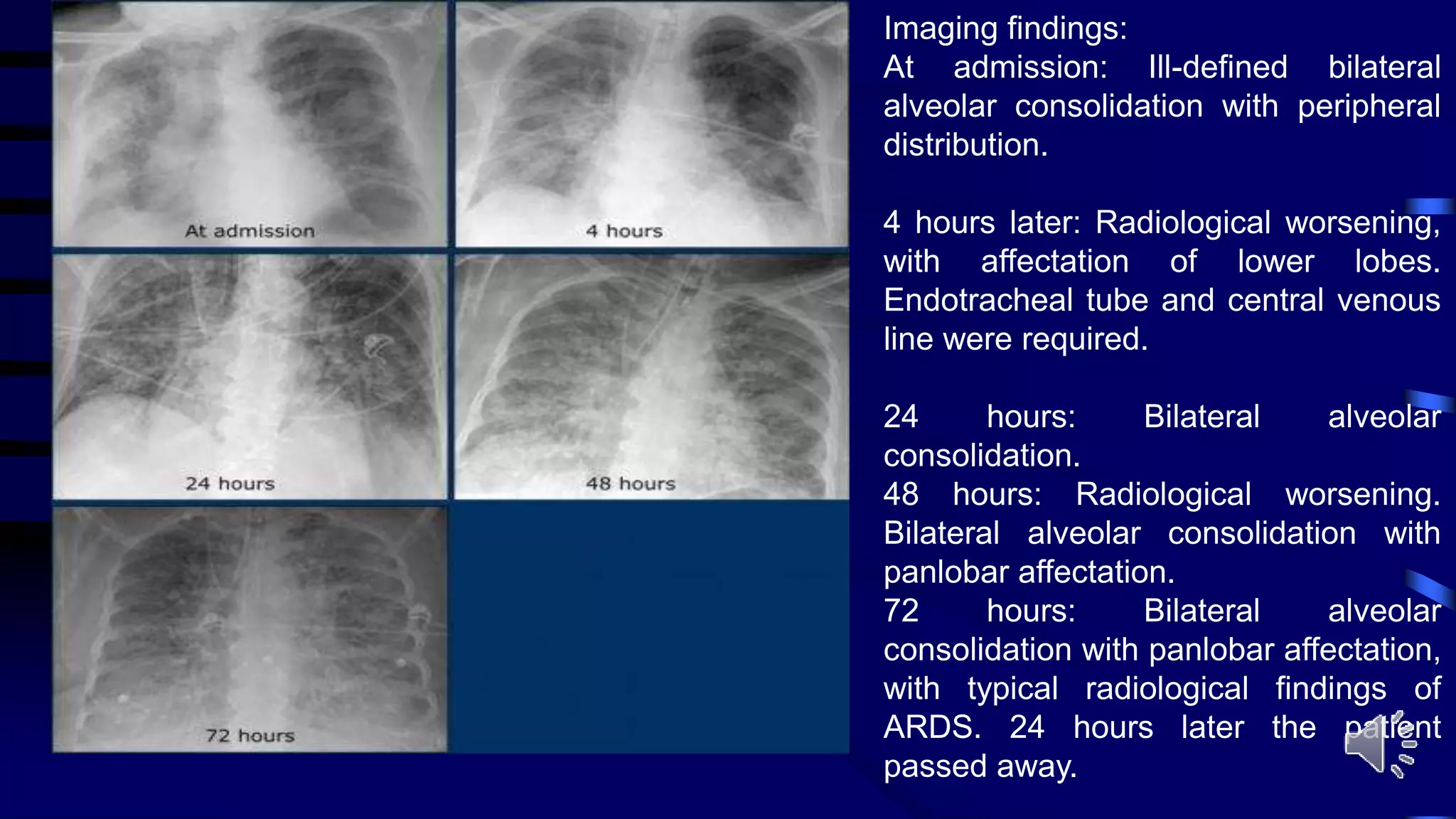
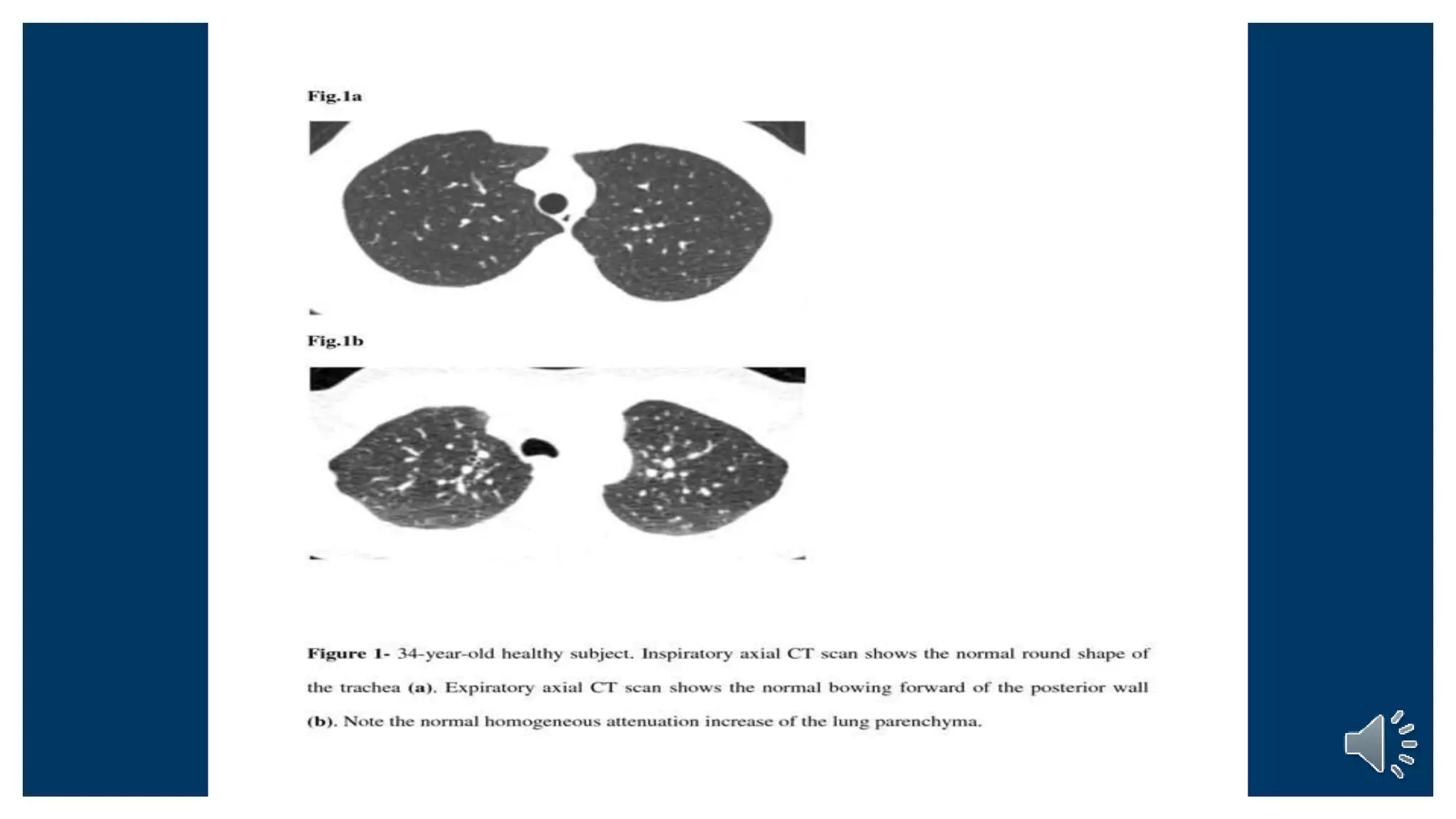
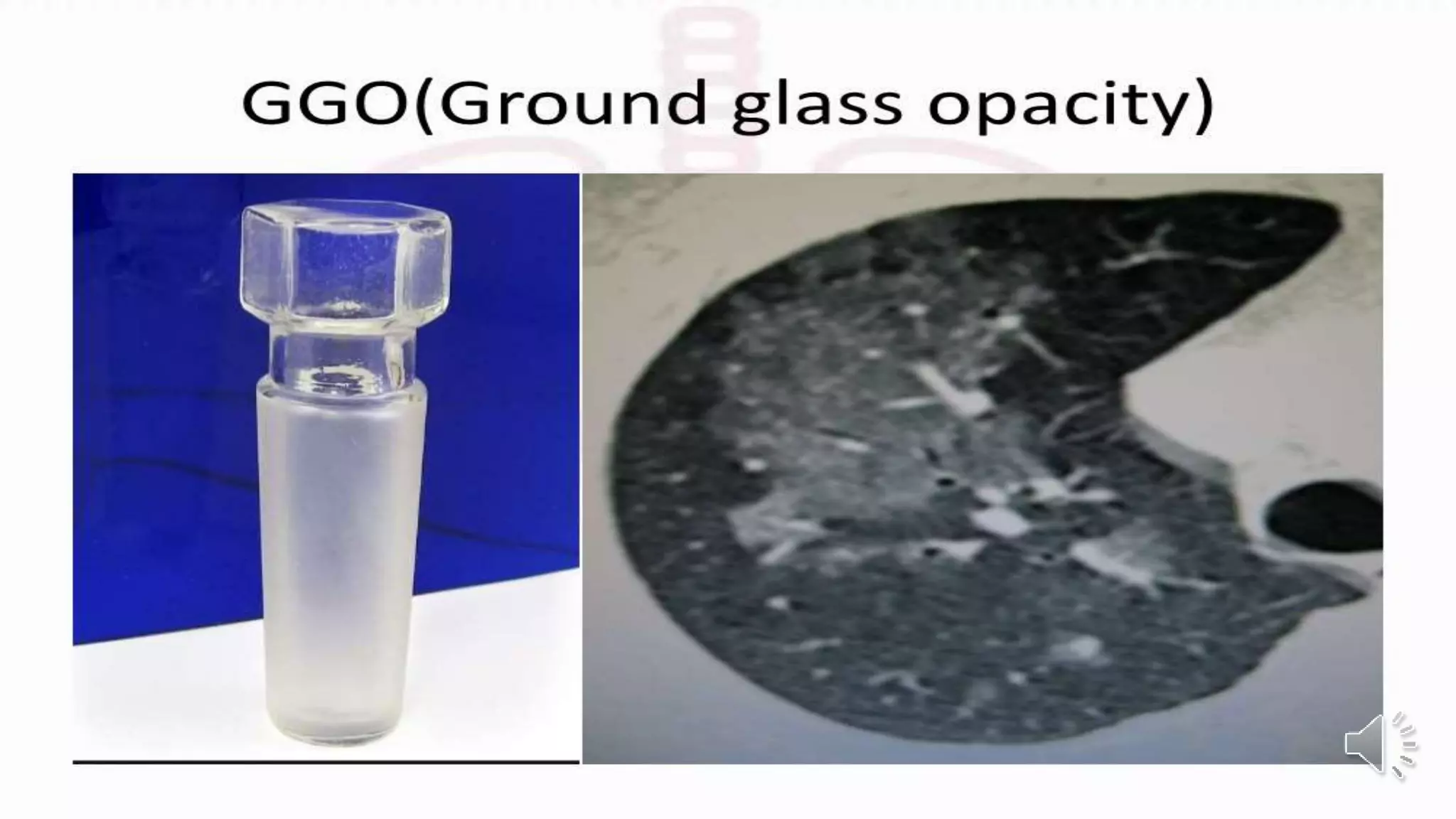
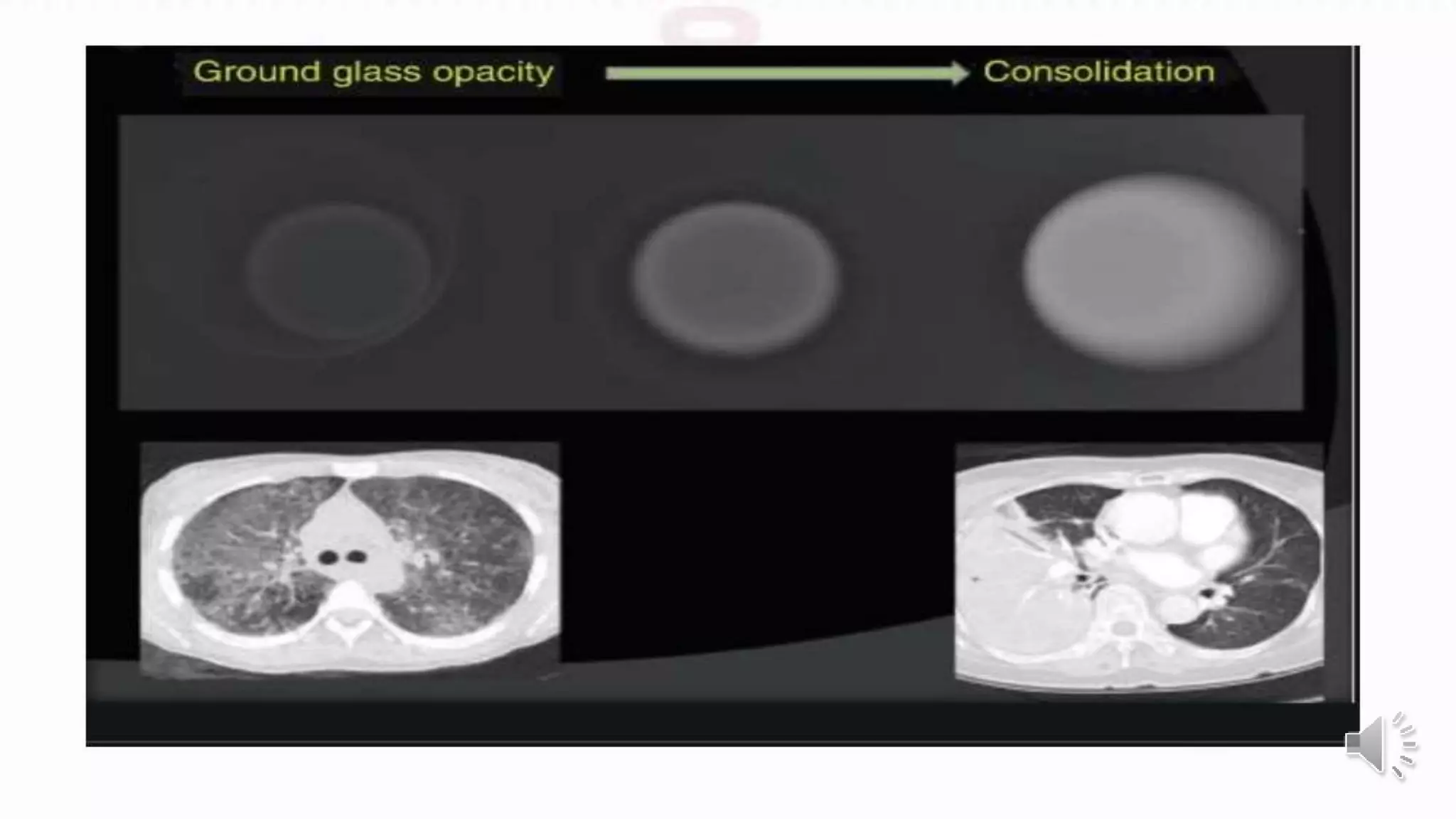
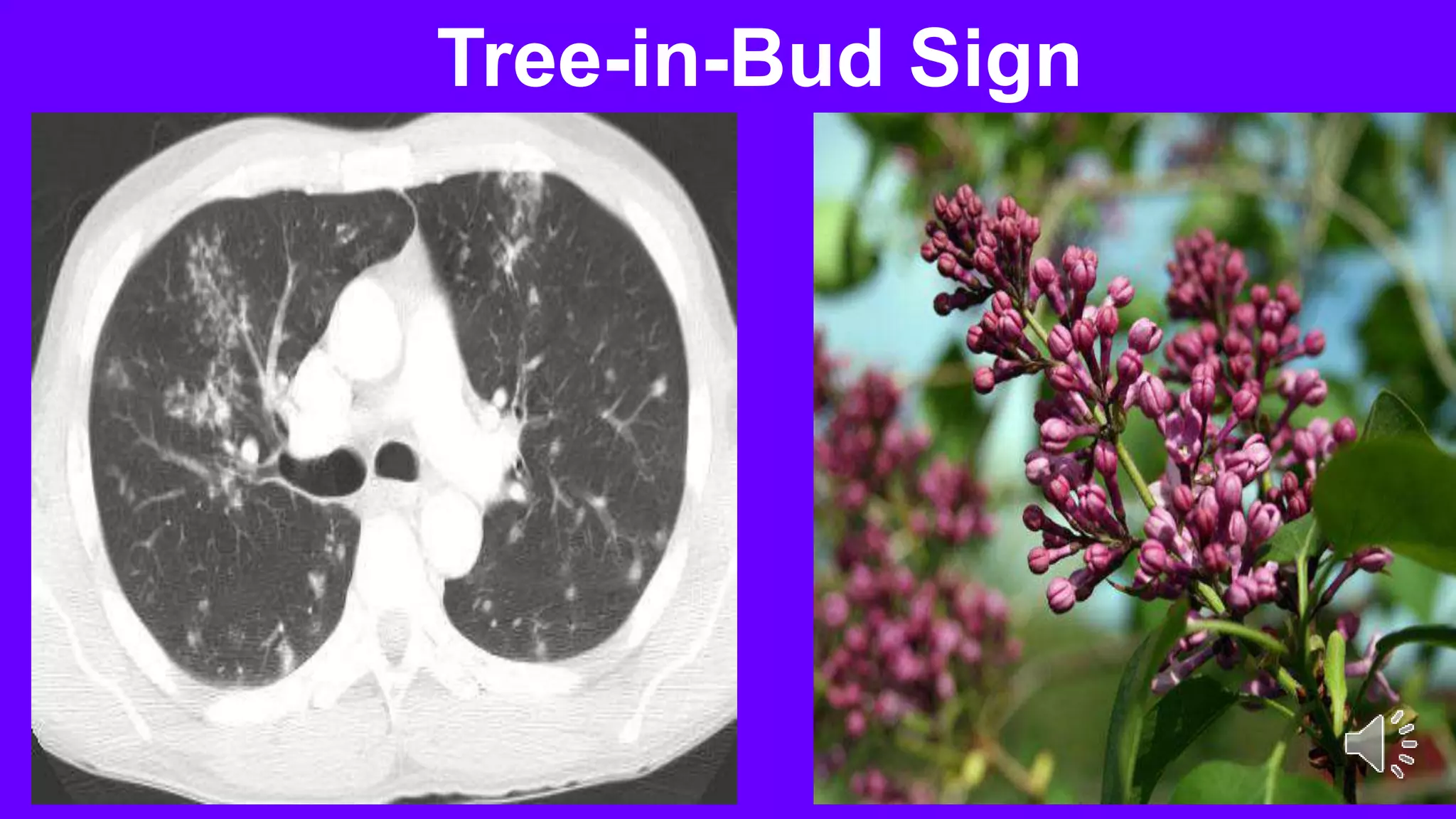
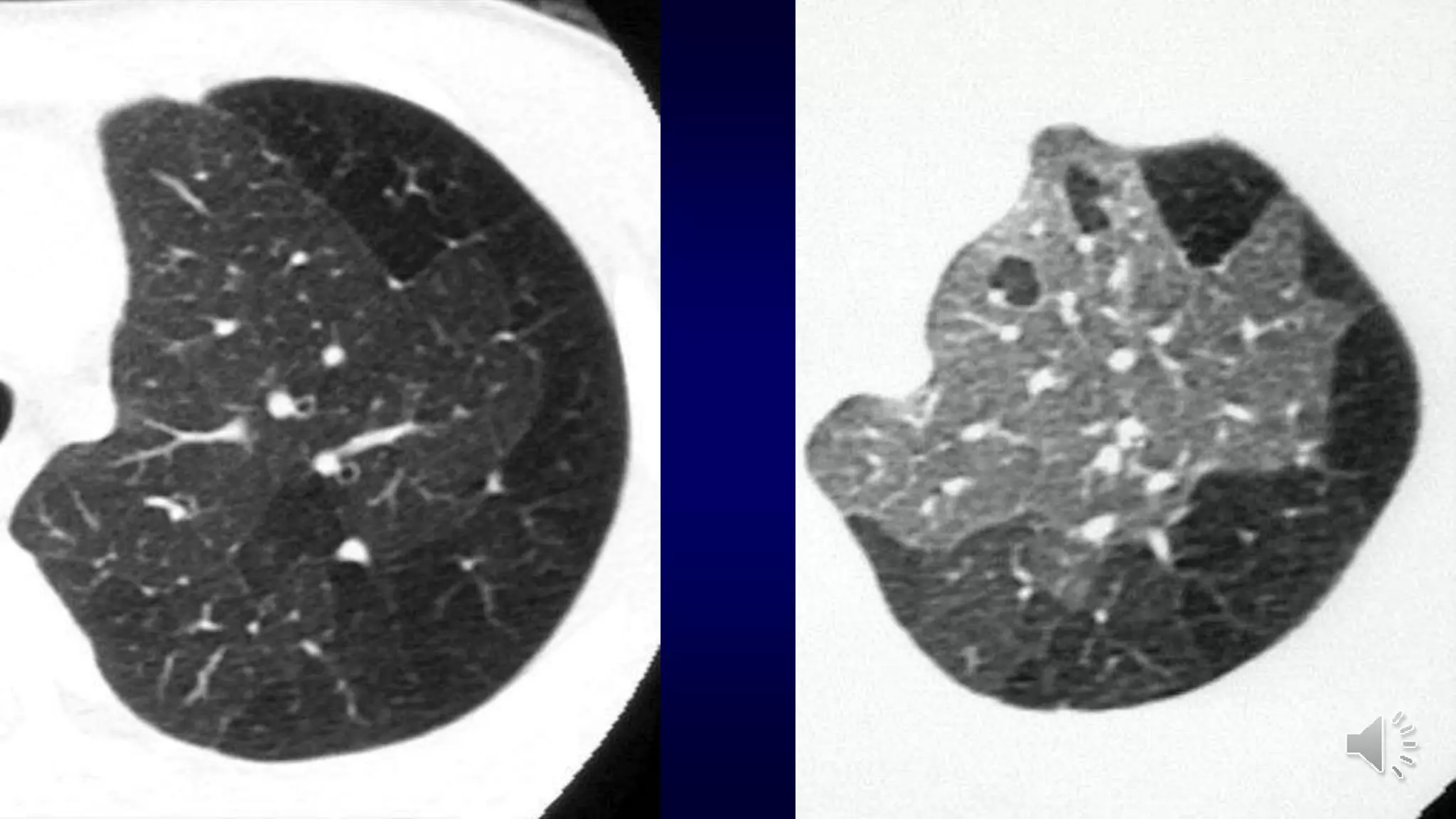
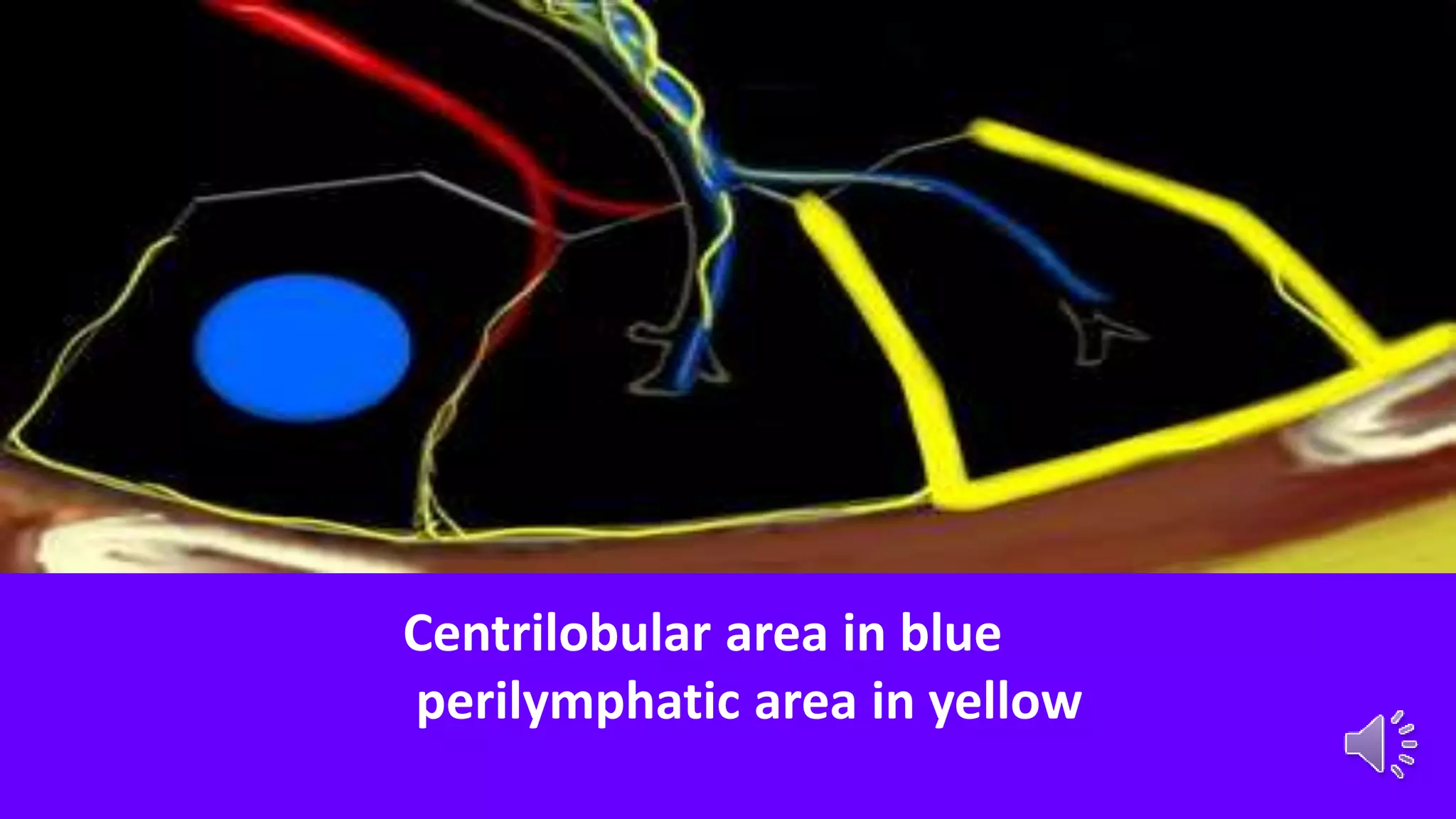
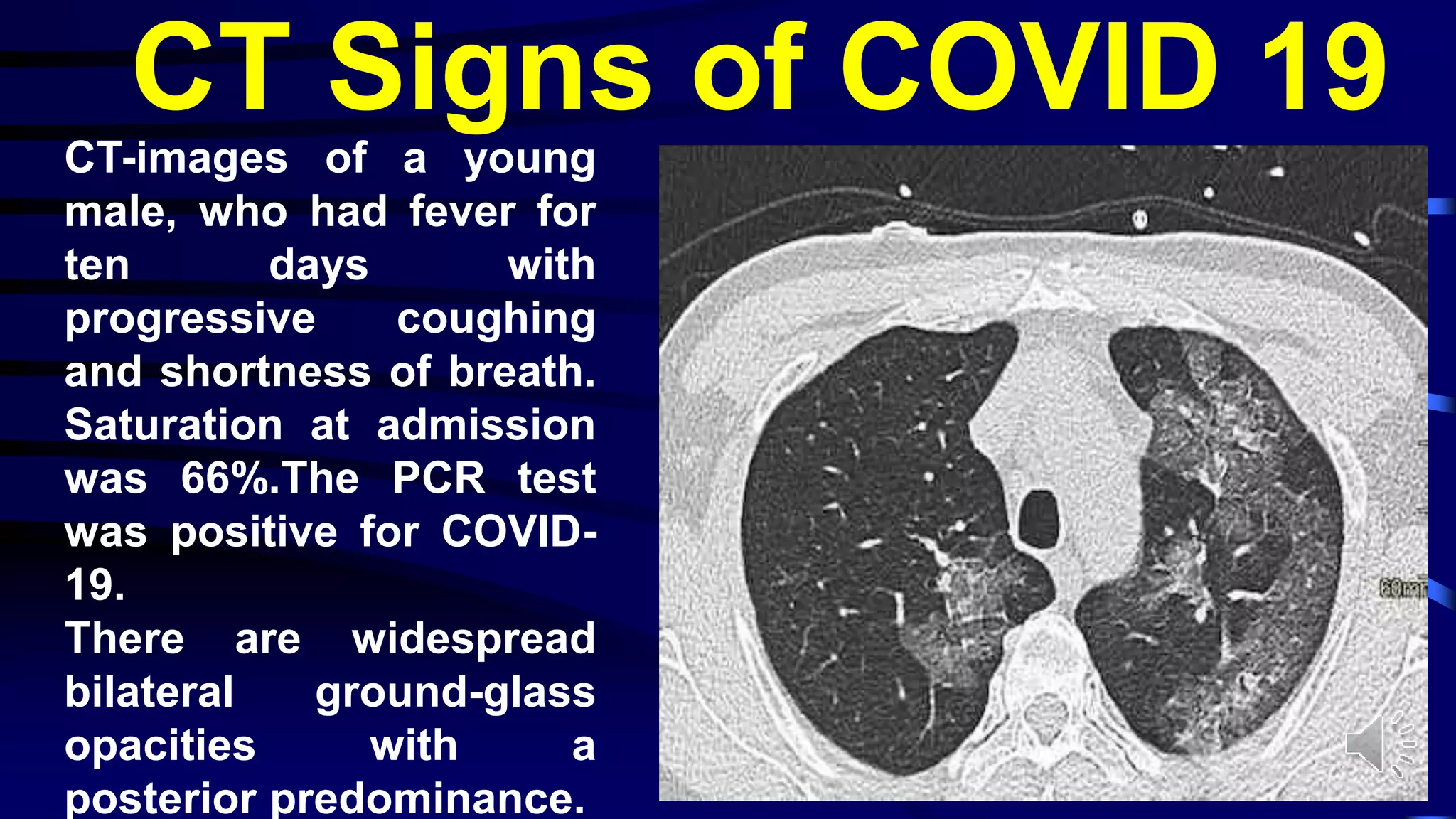
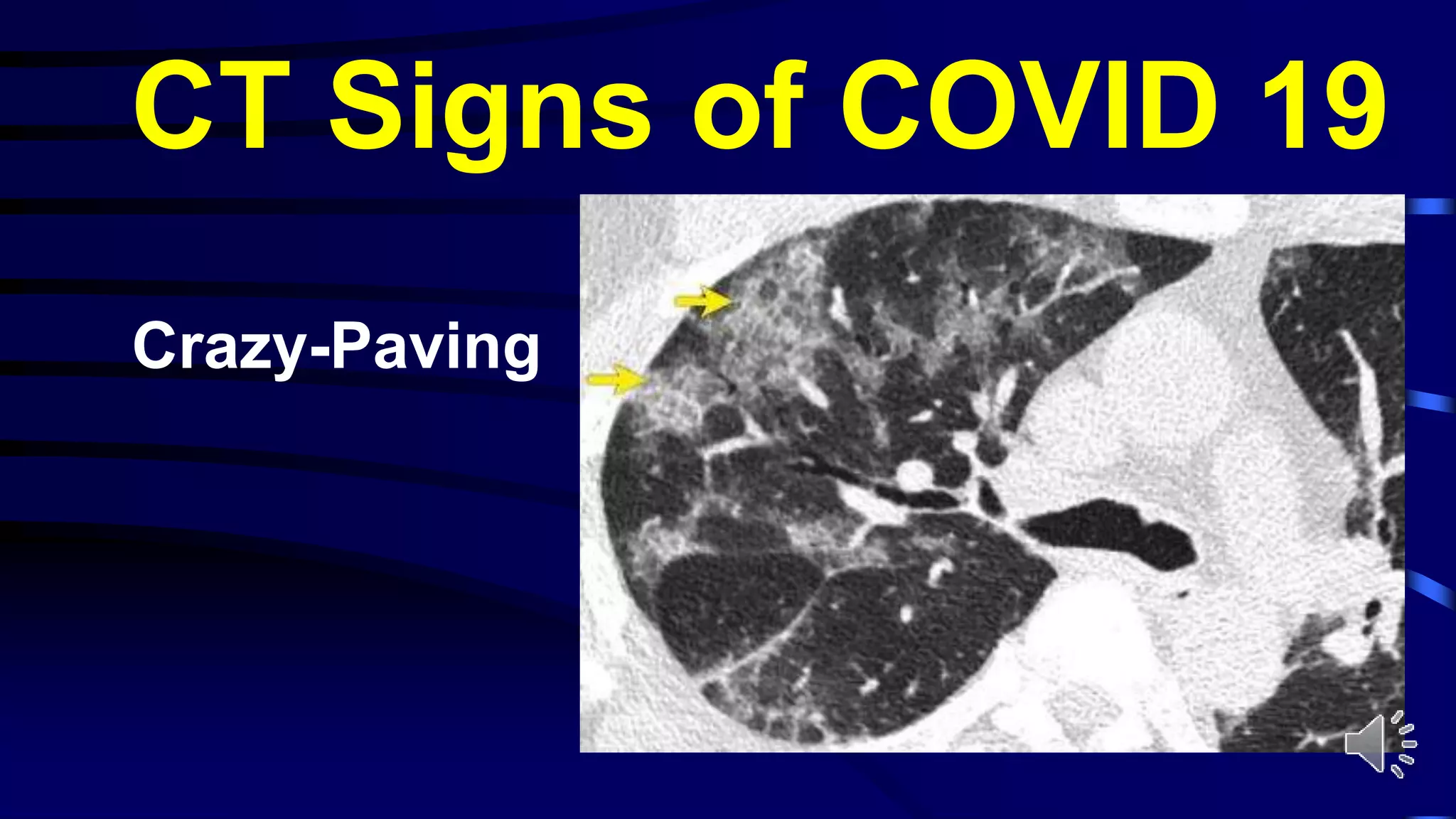
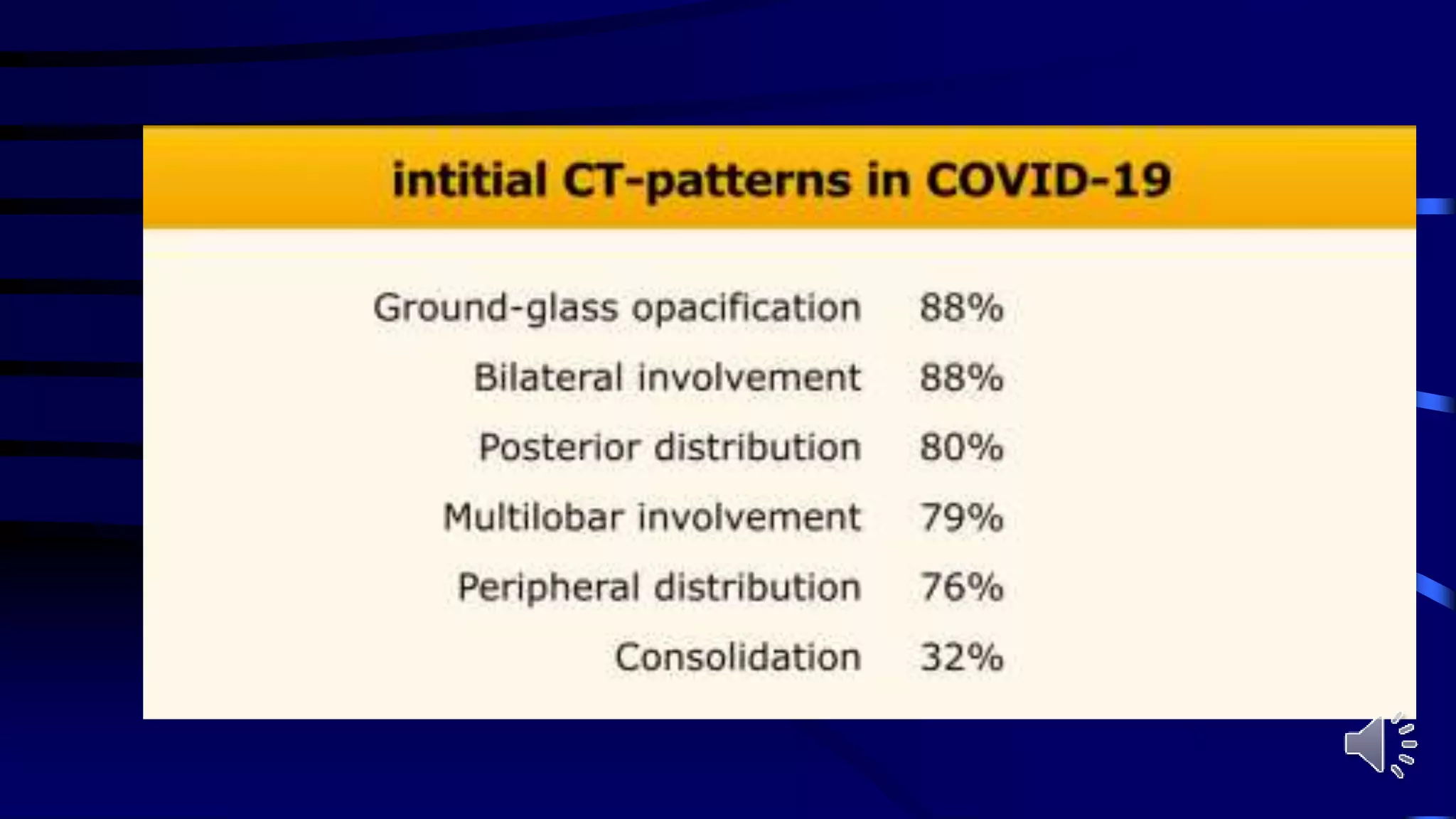
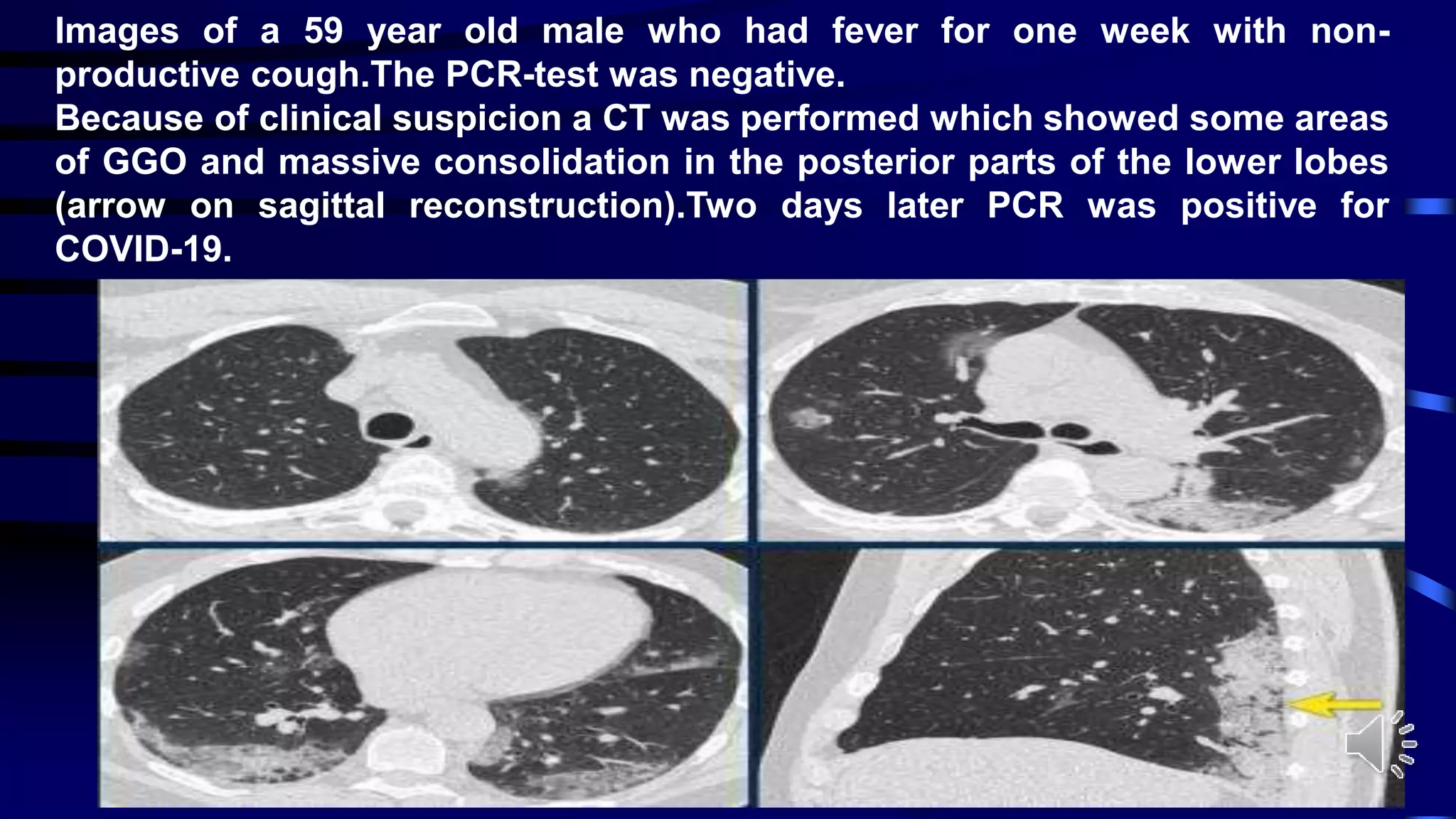
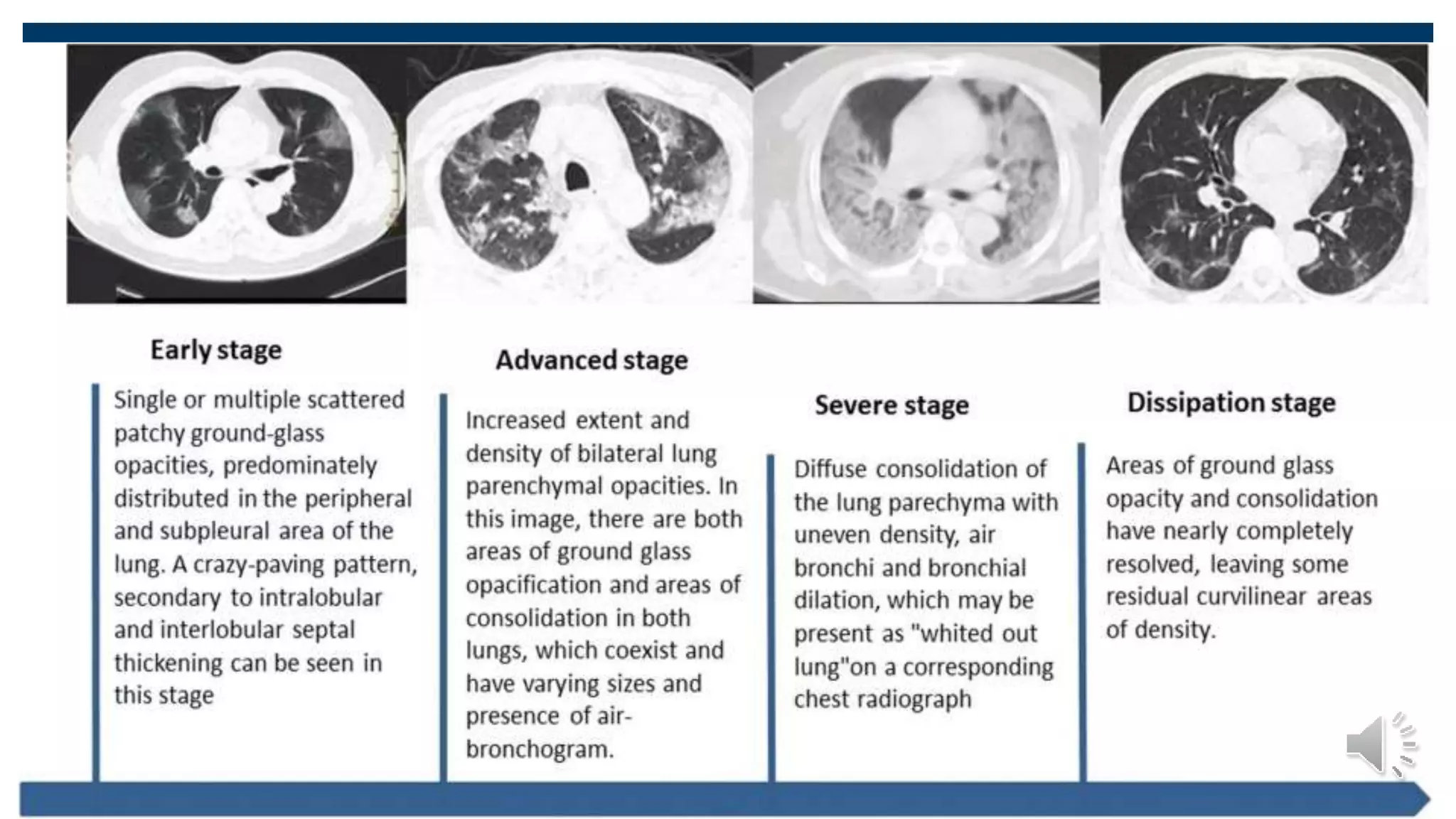
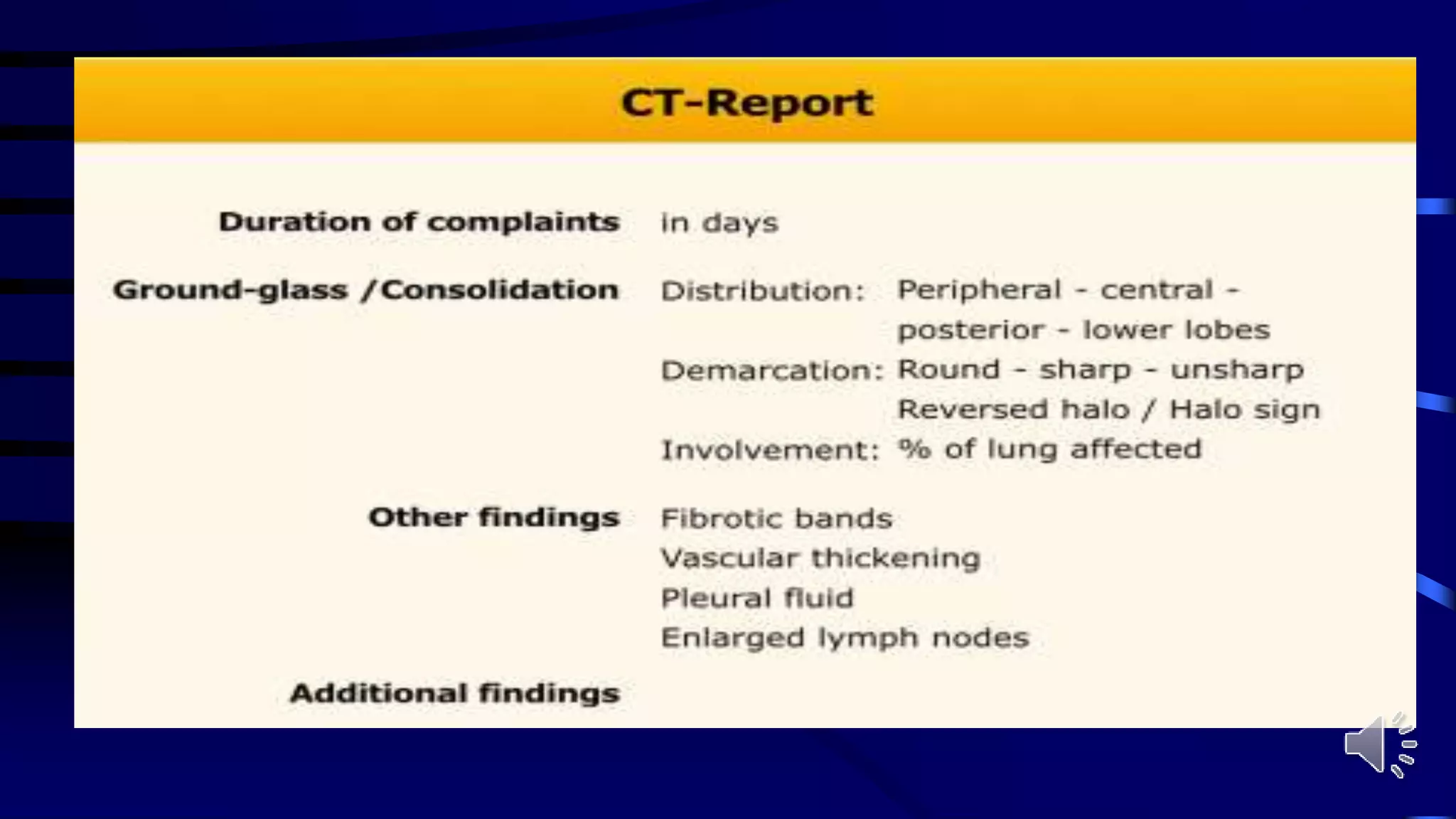
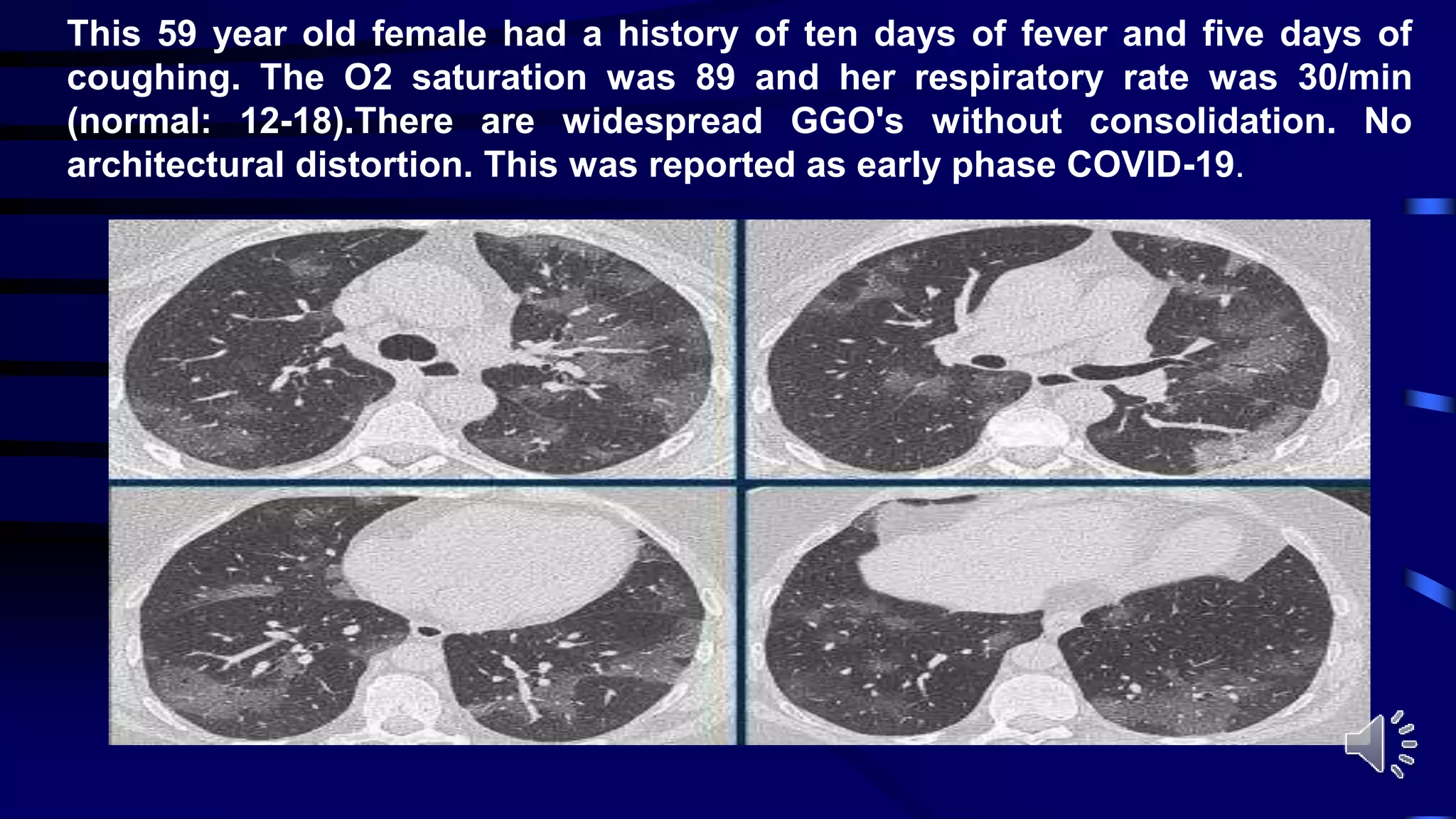
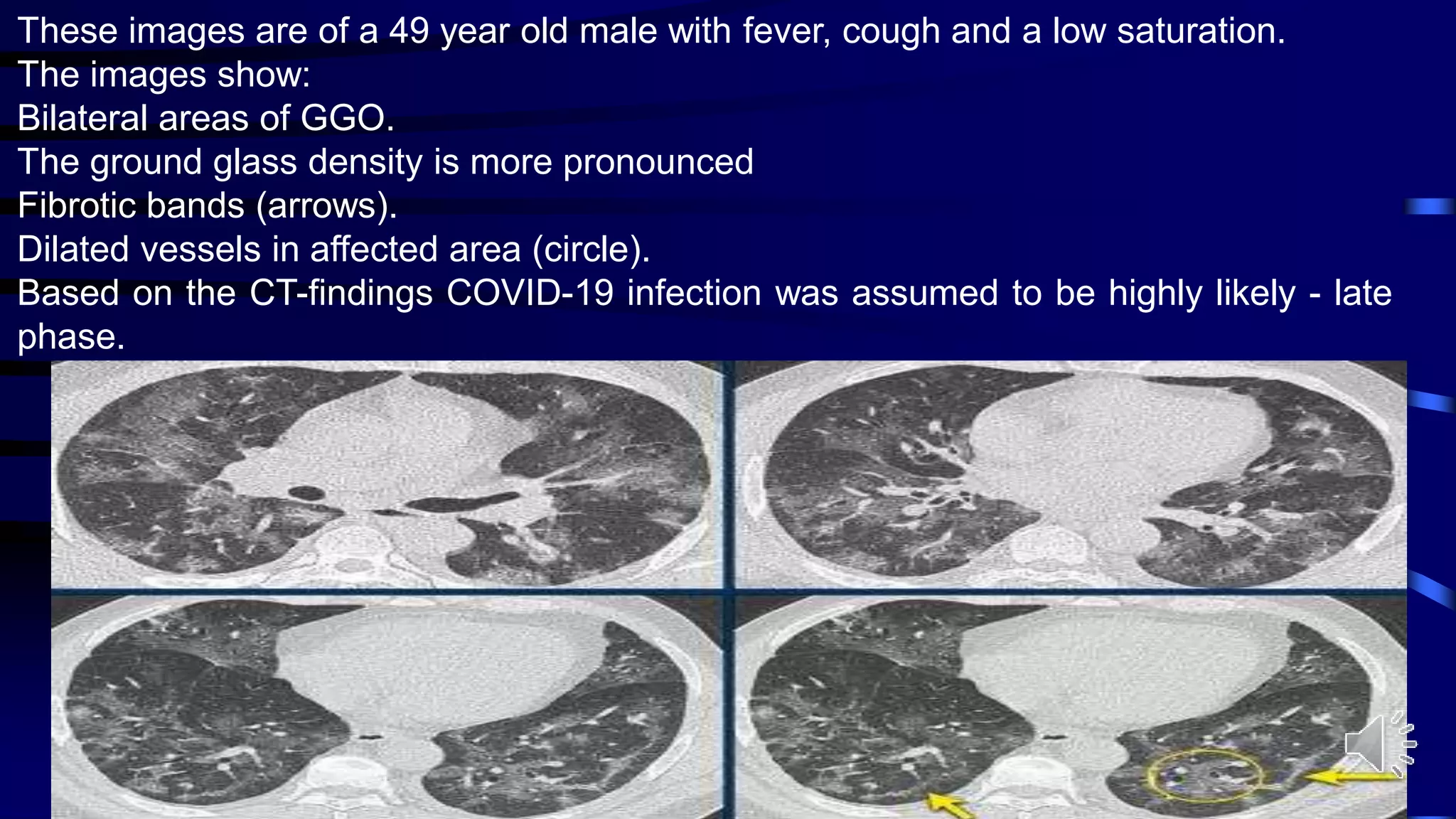
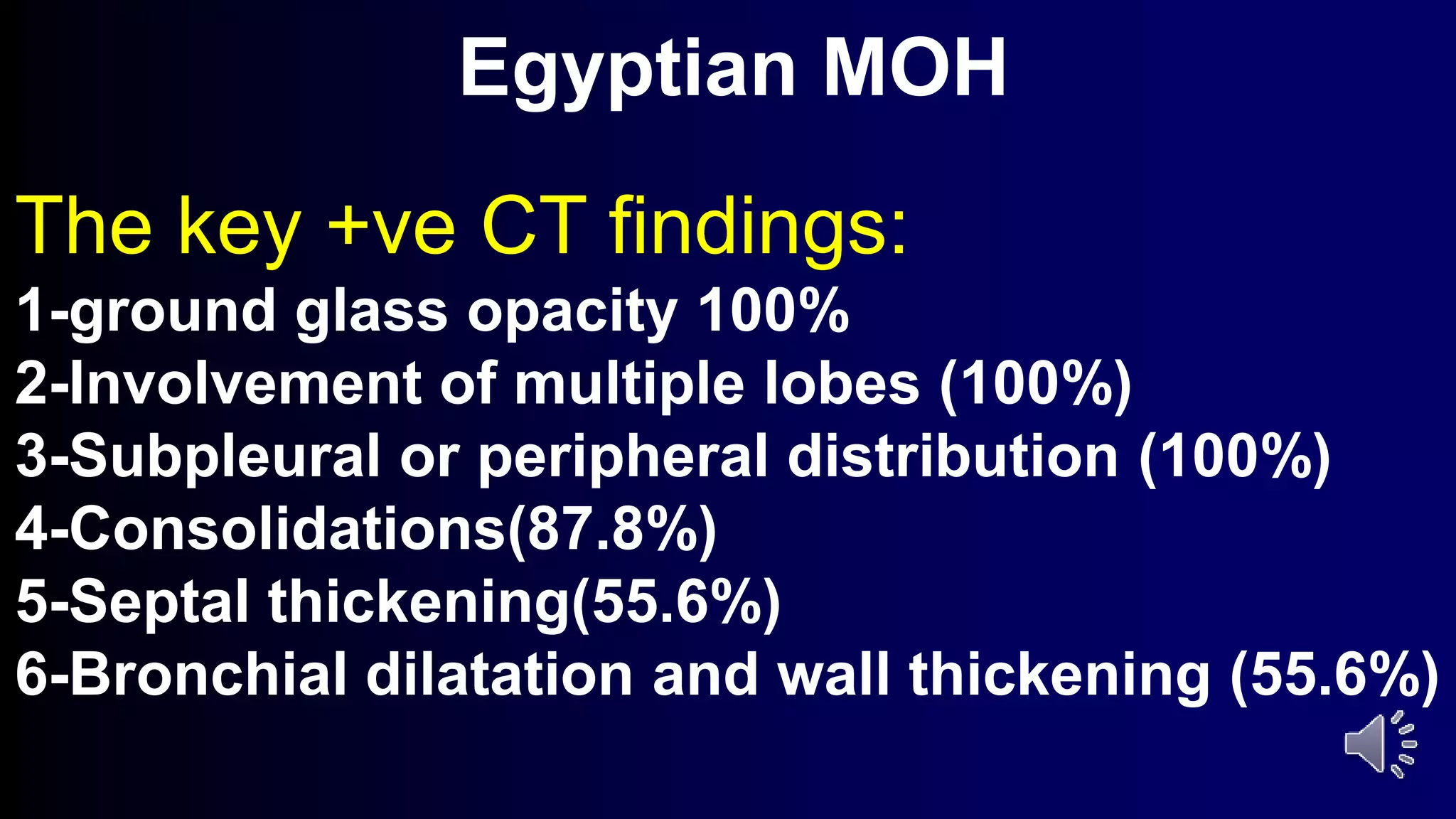
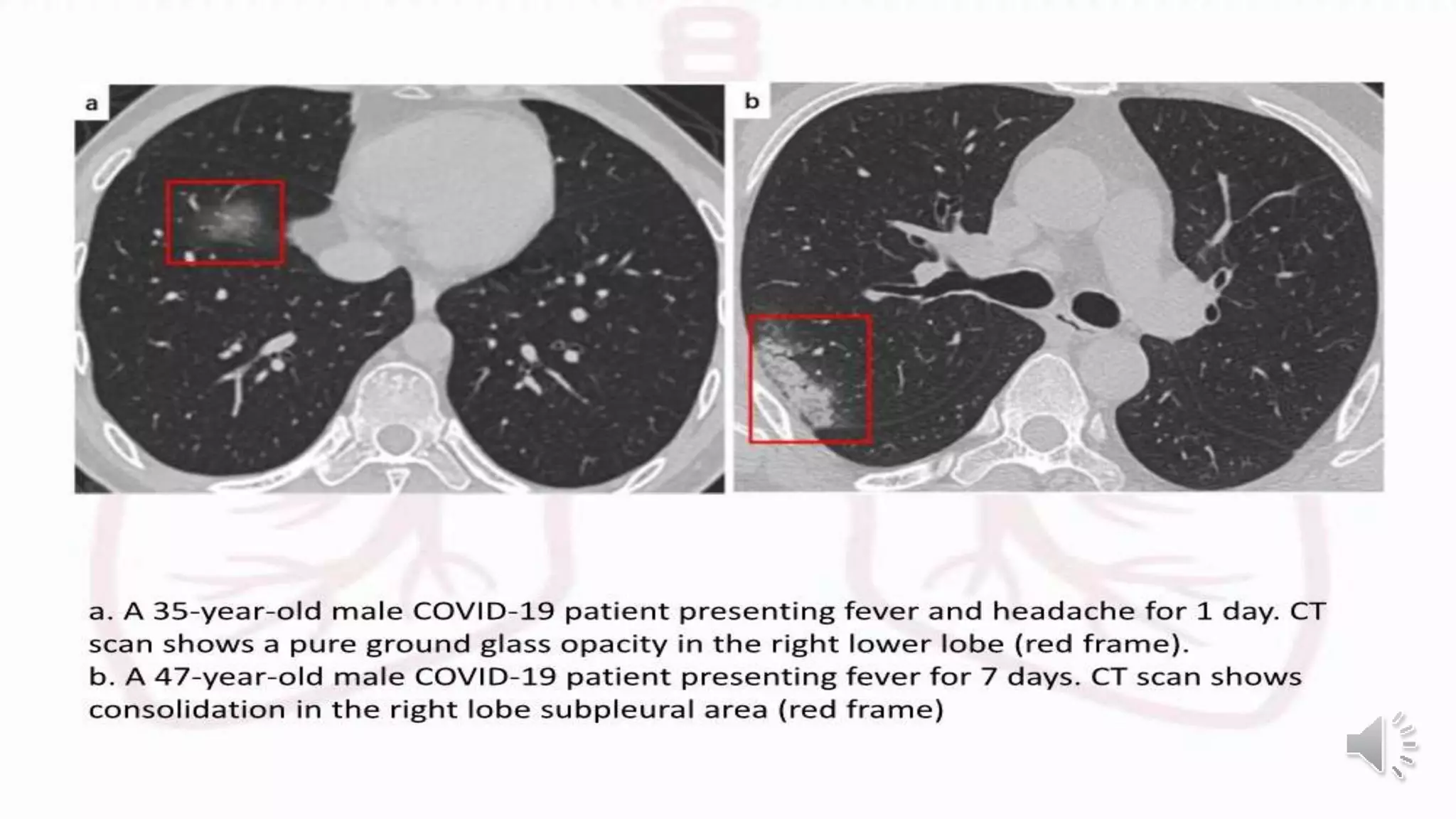
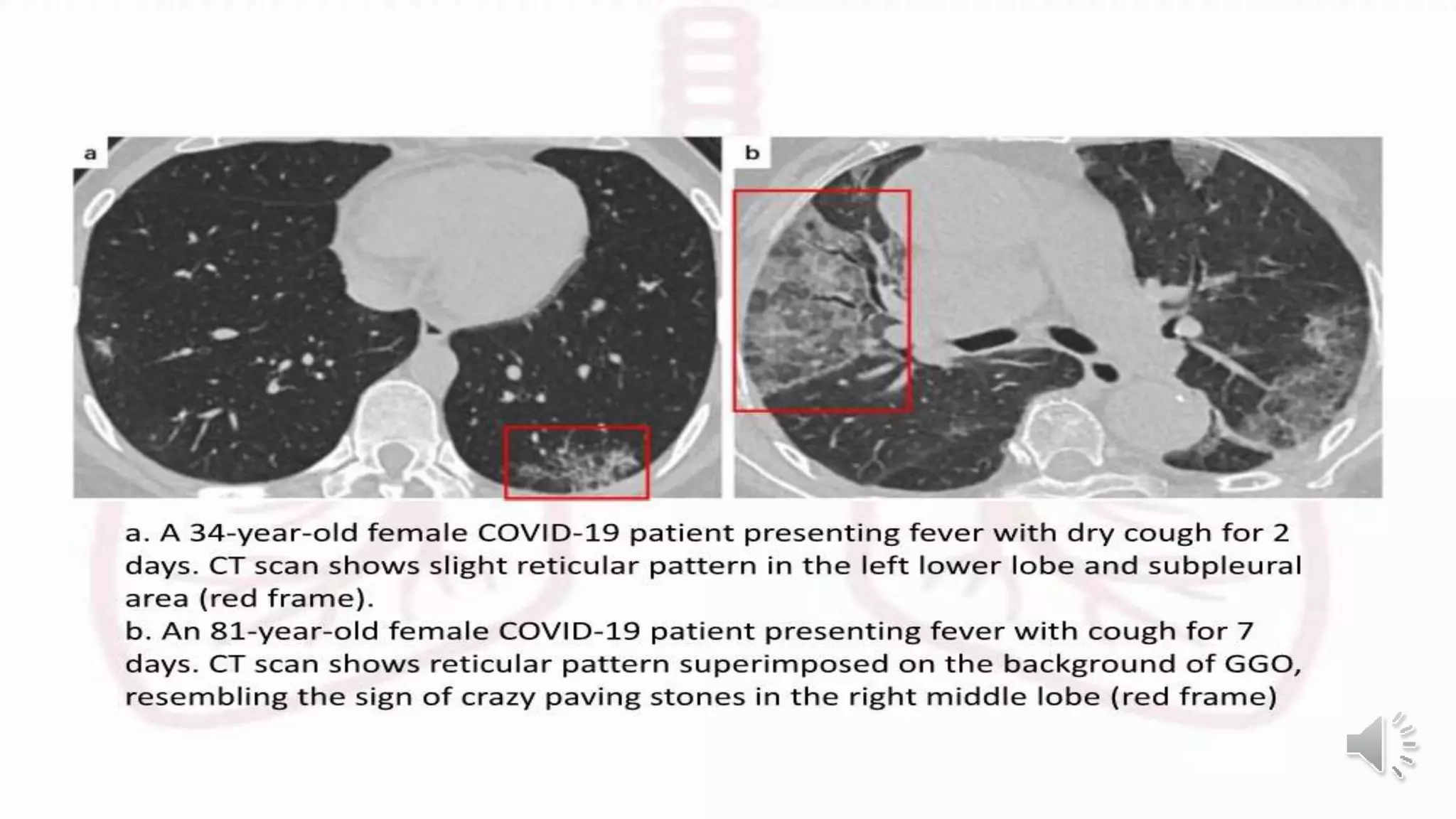
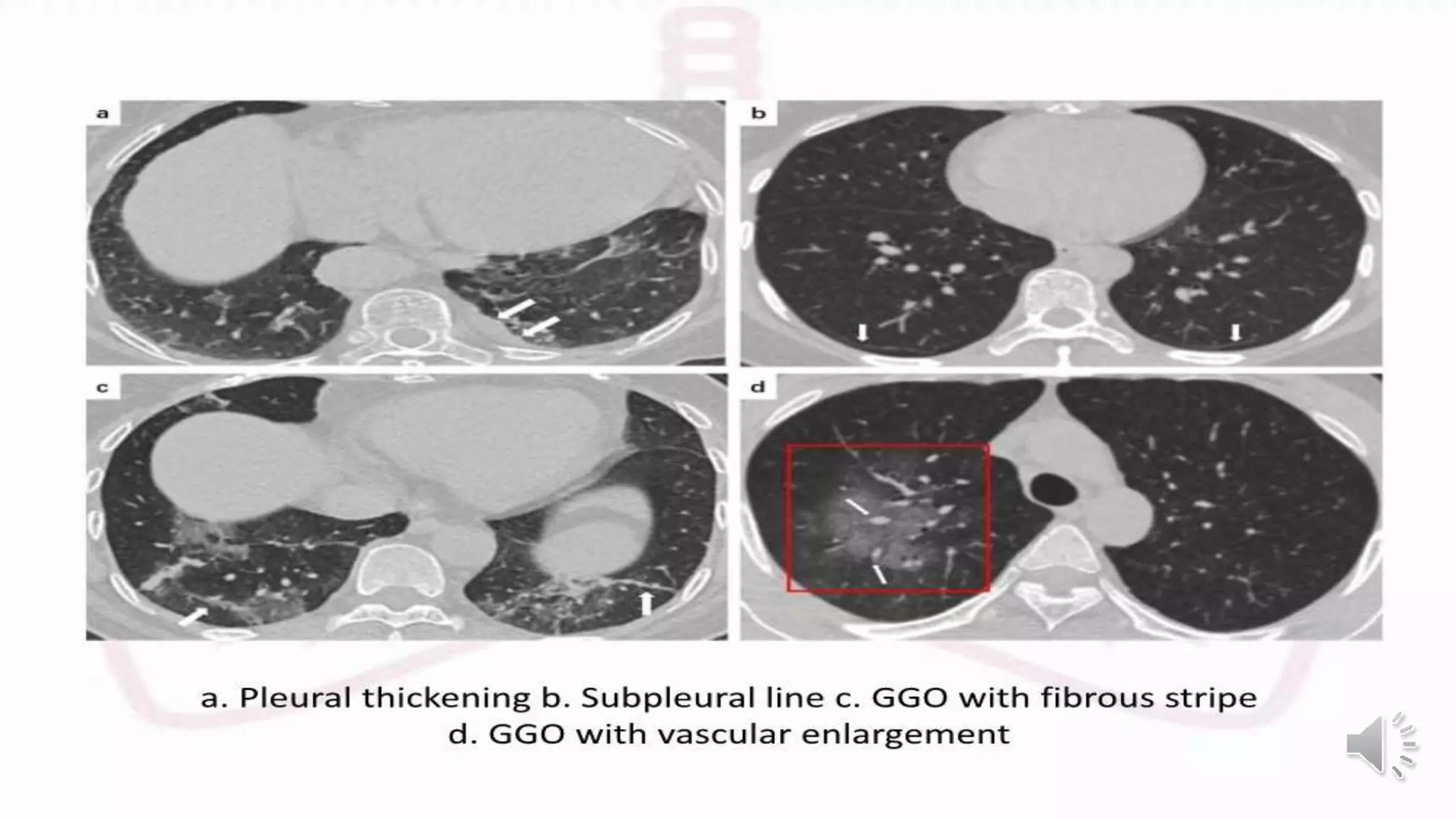
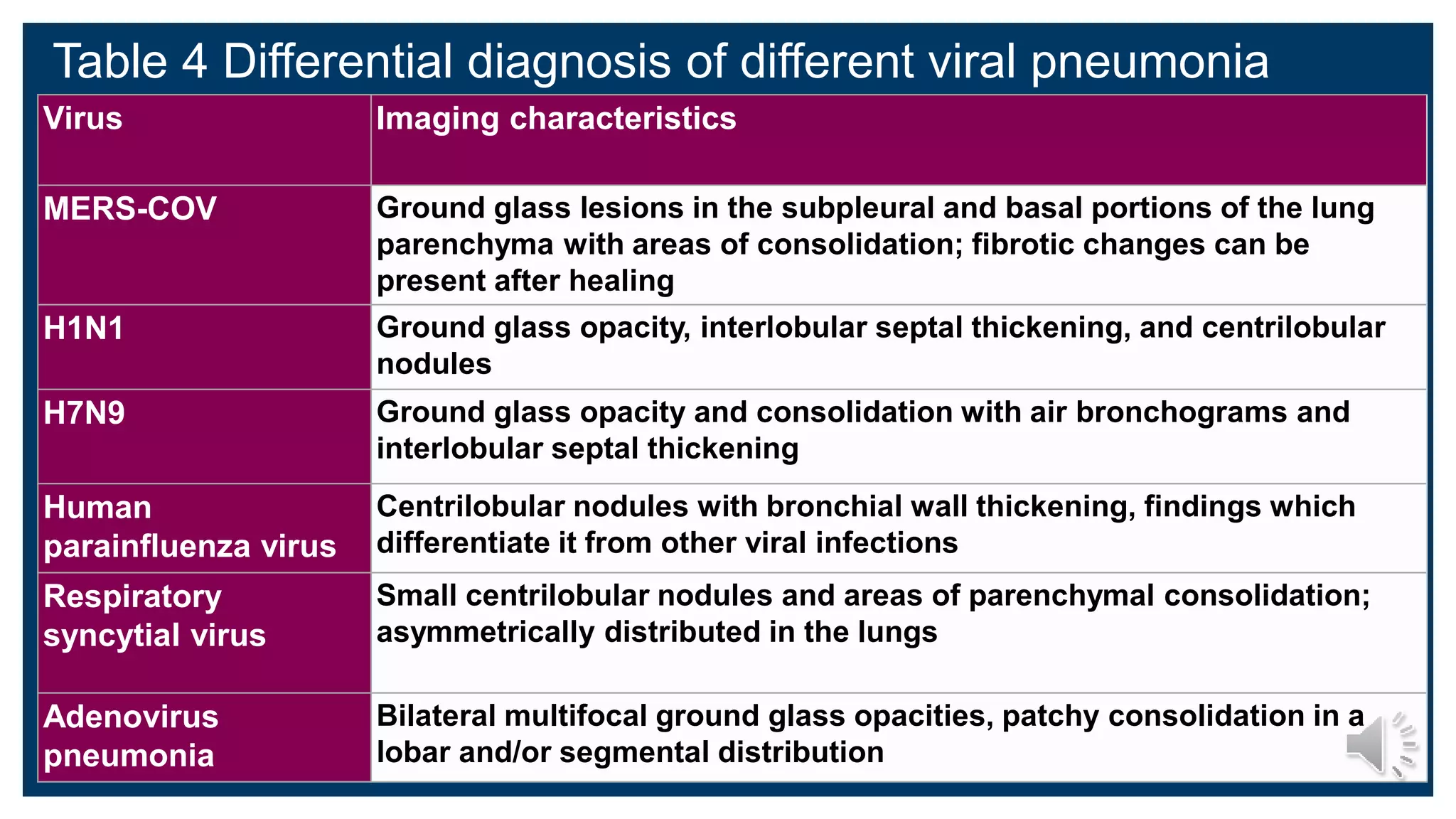
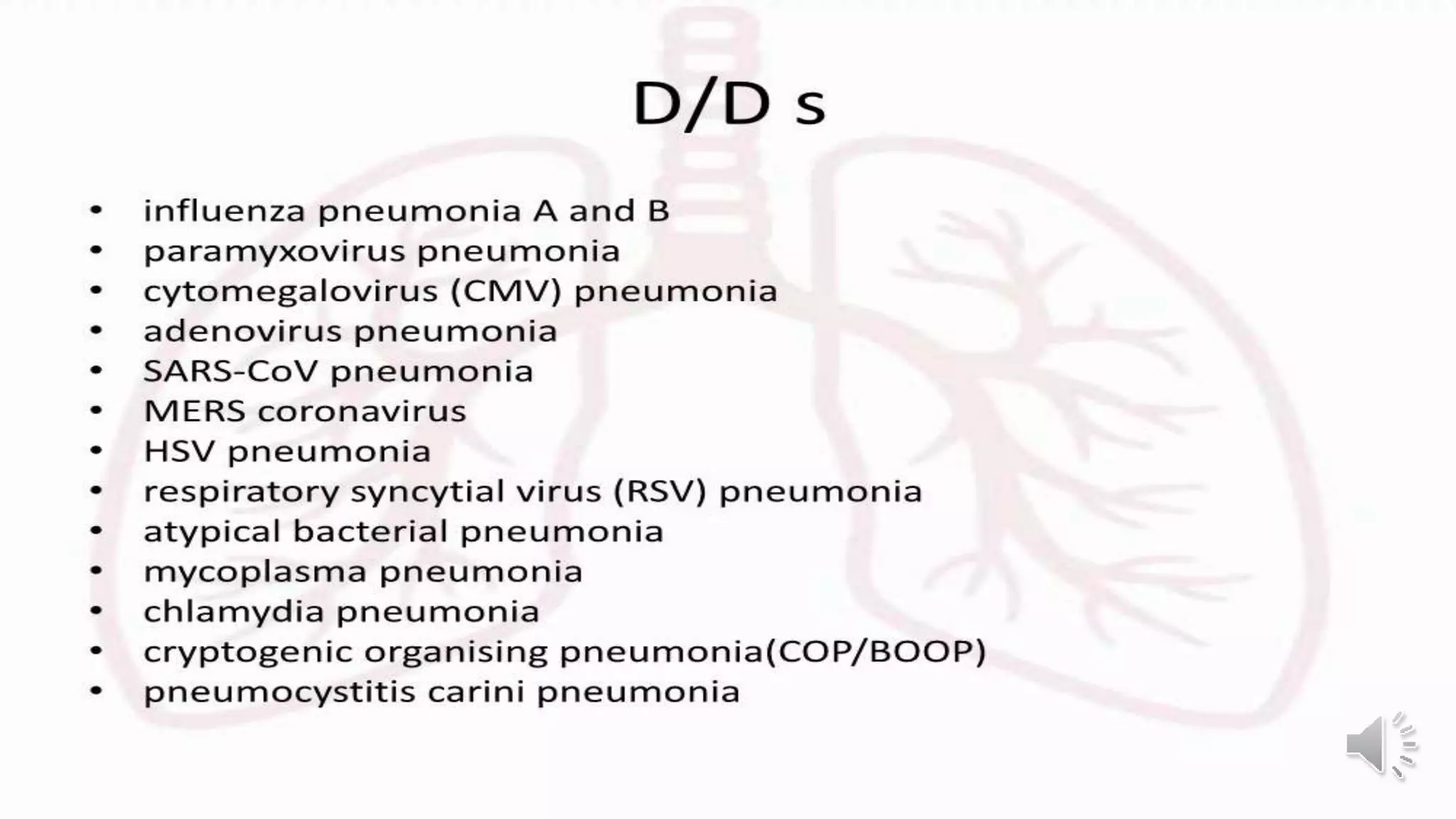
This document provides an overview of the radiological presentation of COVID-19 based on CT scans and chest x-rays. It finds that ground glass opacities are the most common CT finding and often appear bilaterally in the lower lobes in a peripheral or subpleural distribution. Later stages may also show consolidation, septal thickening, and traction bronchiectasis. Chest x-rays are less sensitive than CT early on but can still detect signs of disease progression like bilateral opacities and consolidation. Pediatric cases tend to be milder with fewer abnormal CT findings. The document outlines typical features, frequencies of signs, and comparisons between adult and pediatric presentations.