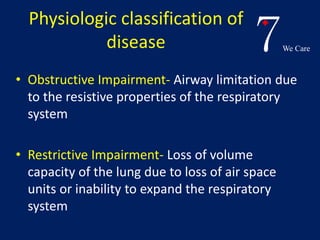
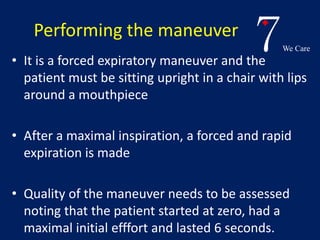
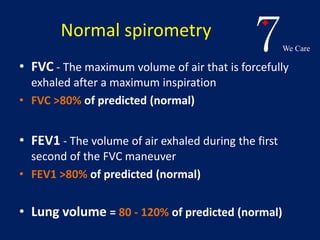
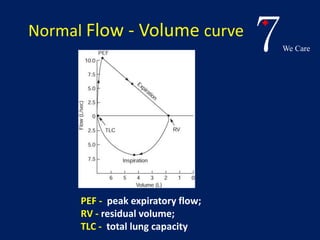
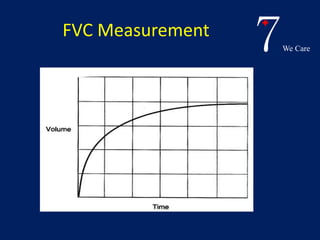
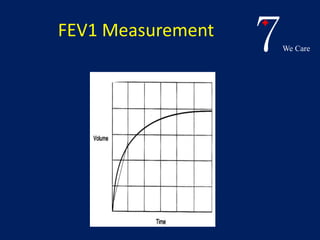
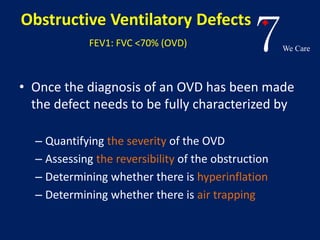
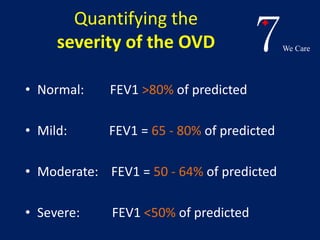
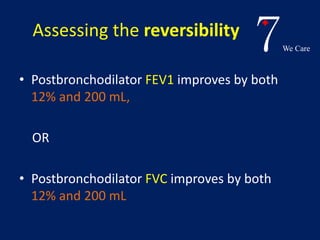
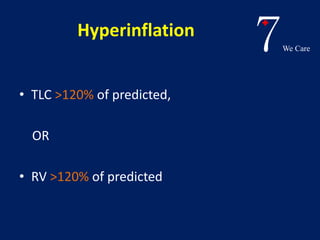
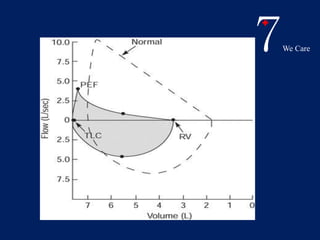
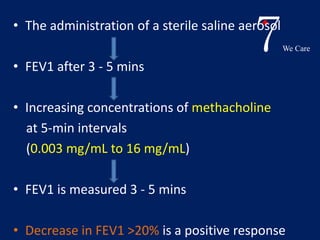
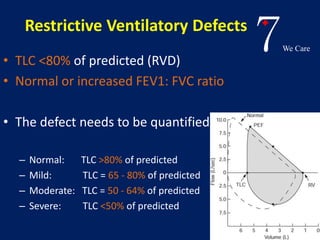
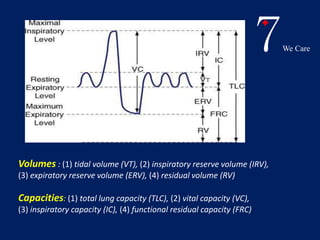
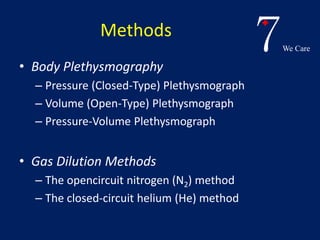
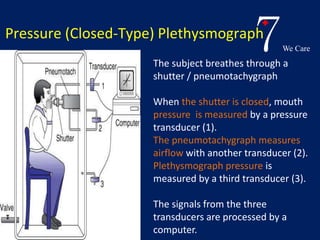
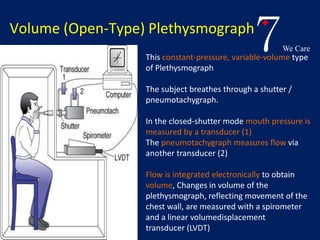
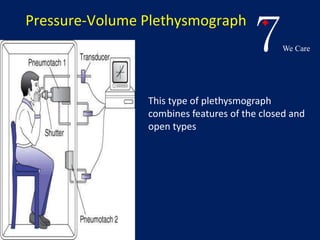
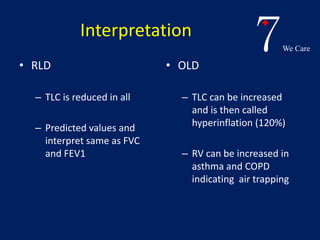
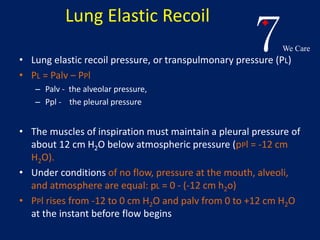
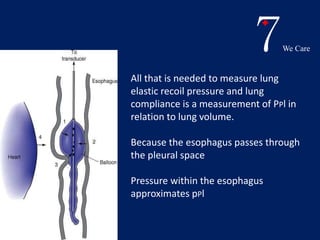
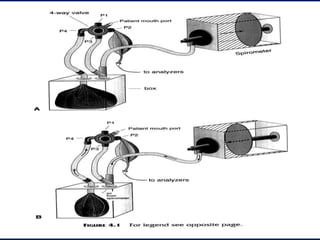
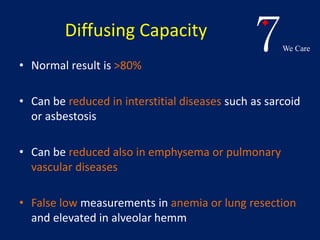
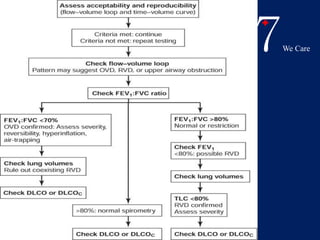
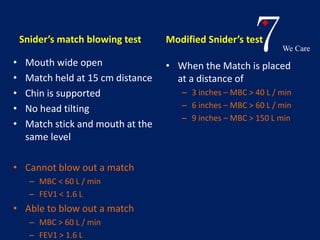
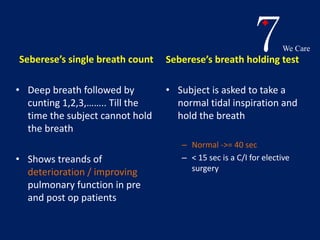
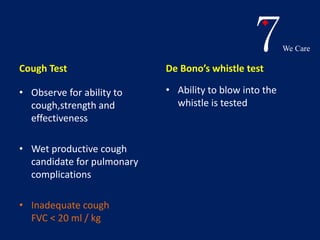
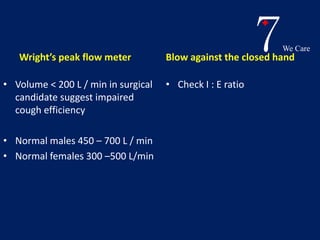
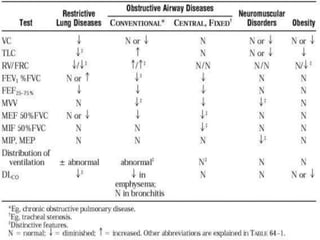
Pulmonary function tests provide objective assessments of respiratory symptoms and can help diagnose respiratory diseases. Spirometry is the most widely used test and measures volumes like FVC and FEV1. Restrictive diseases reduce total lung capacity while obstructive diseases cause decreased FEV1/FVC ratio. Other tests include lung volume measurements using plethysmography or gas dilution, diffusing capacity to assess gas exchange, and methacholine challenge for asthma diagnosis. Bedside tests can also help evaluate respiratory function.