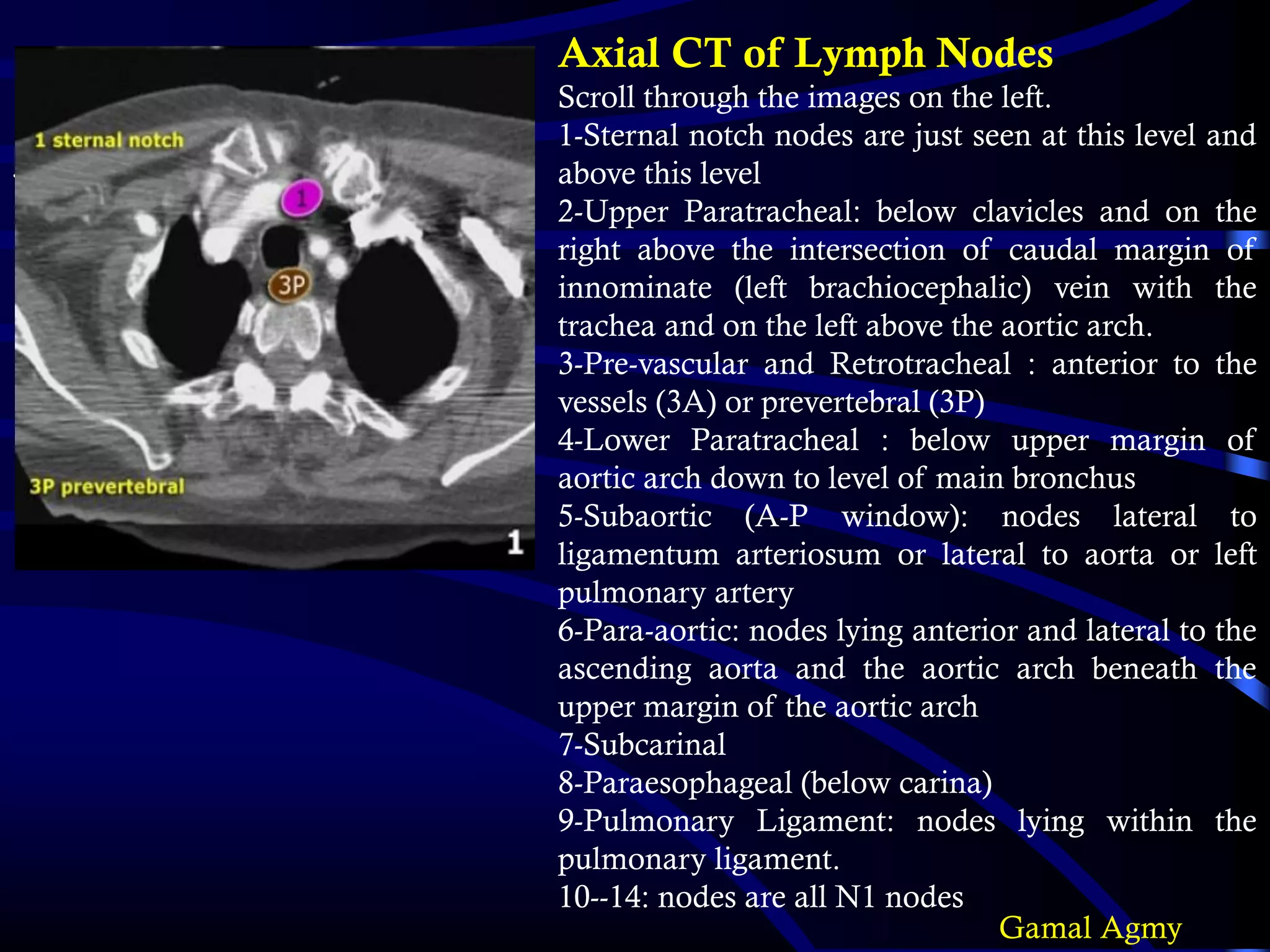
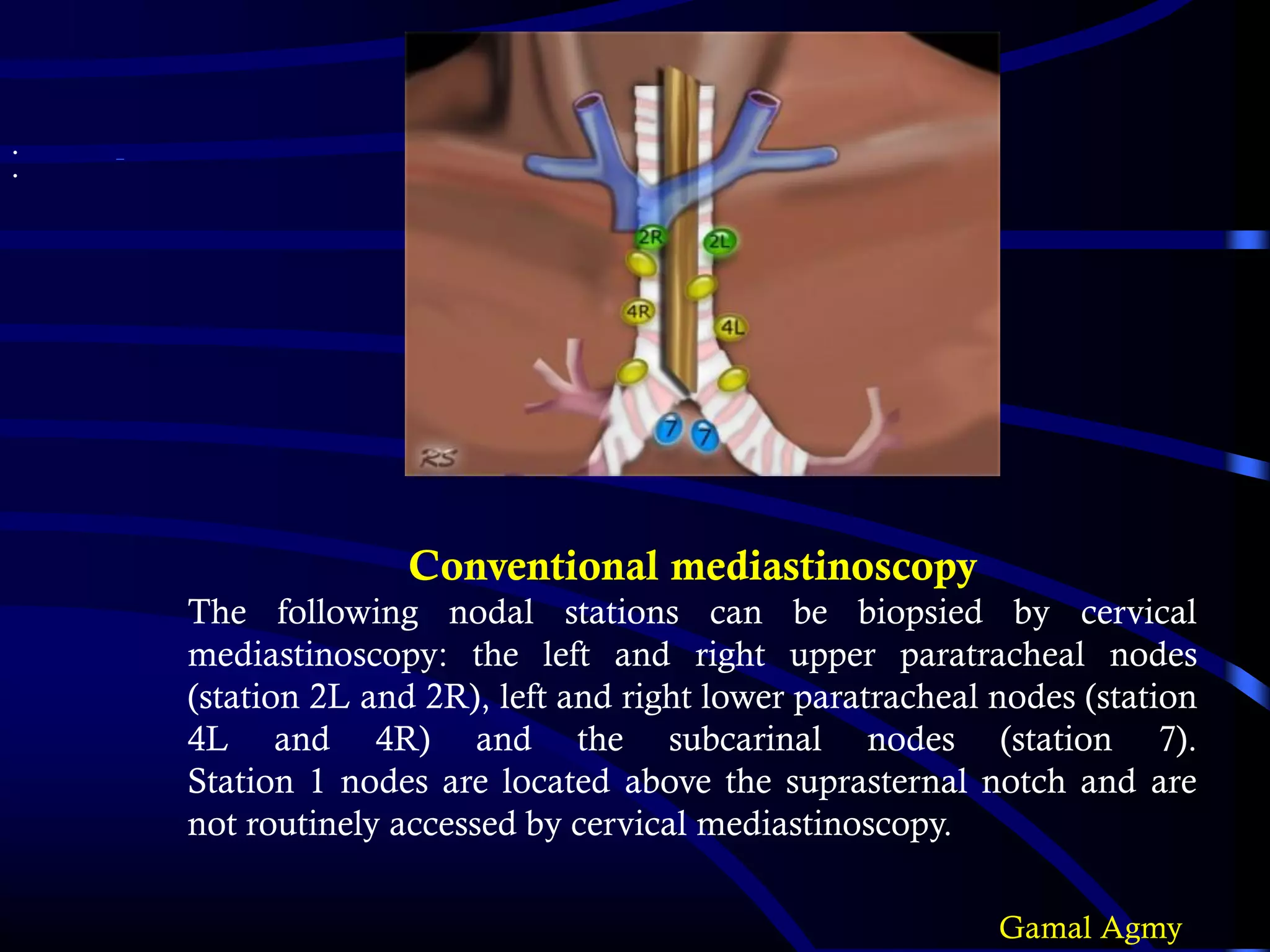
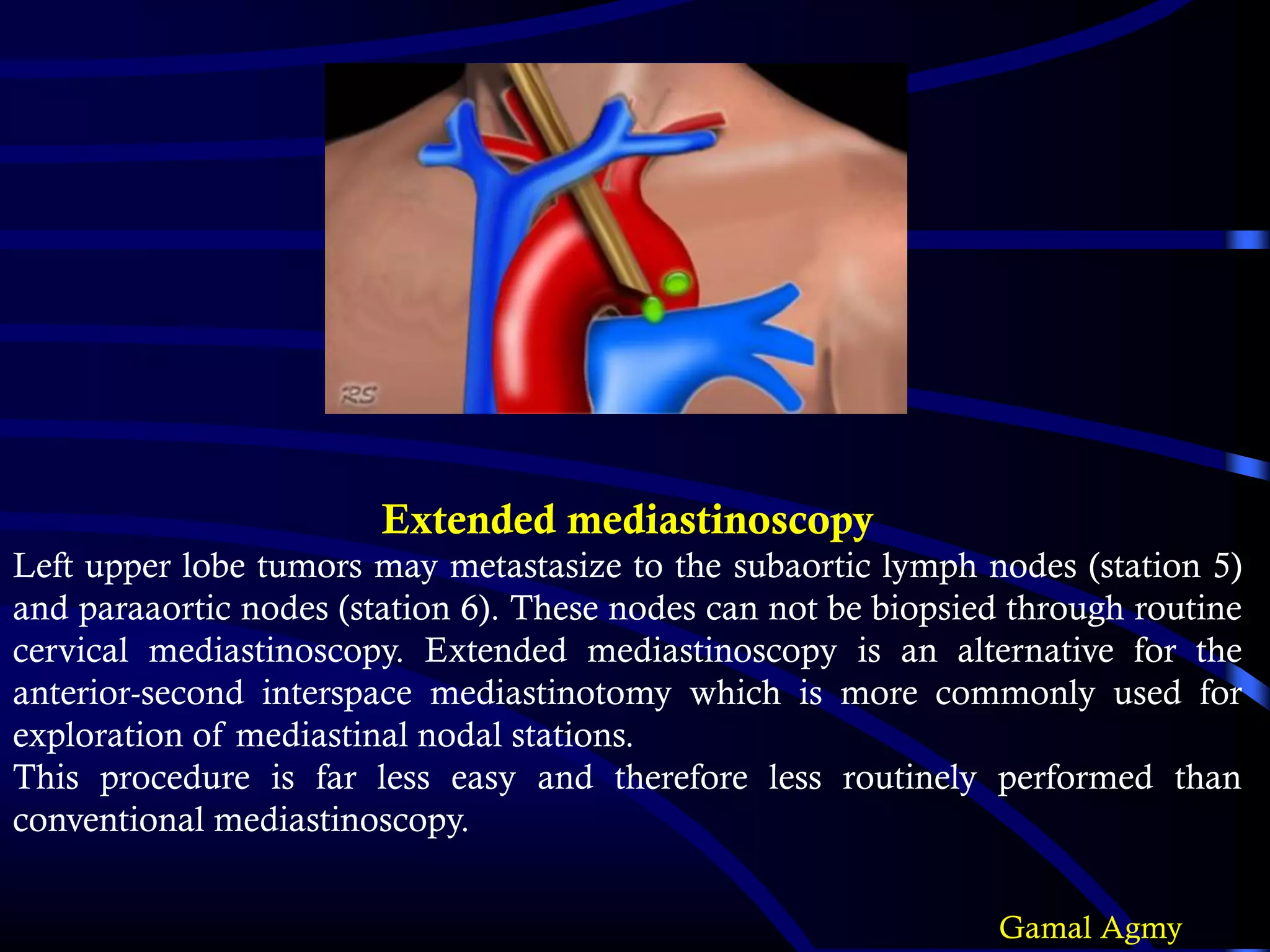
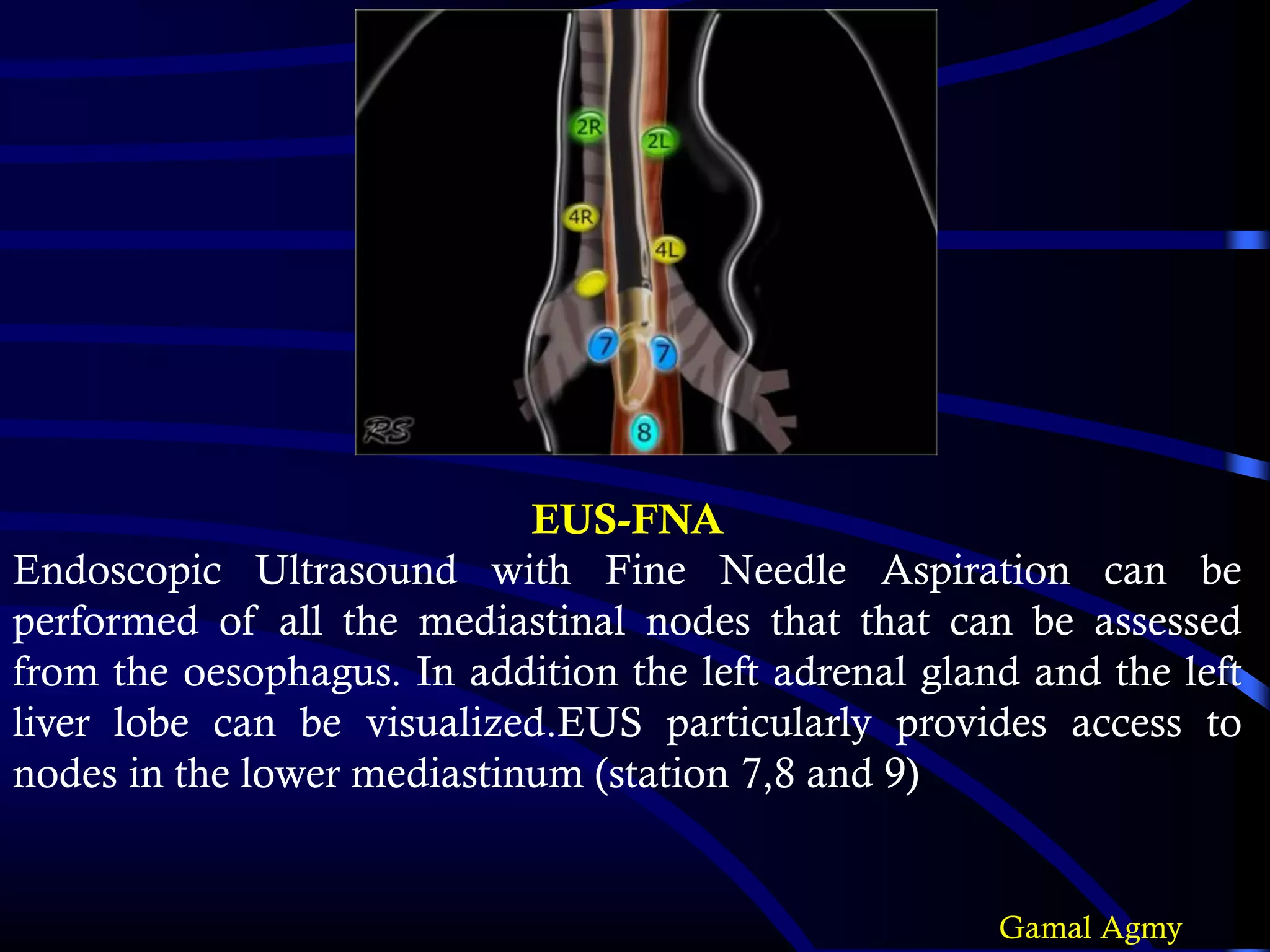
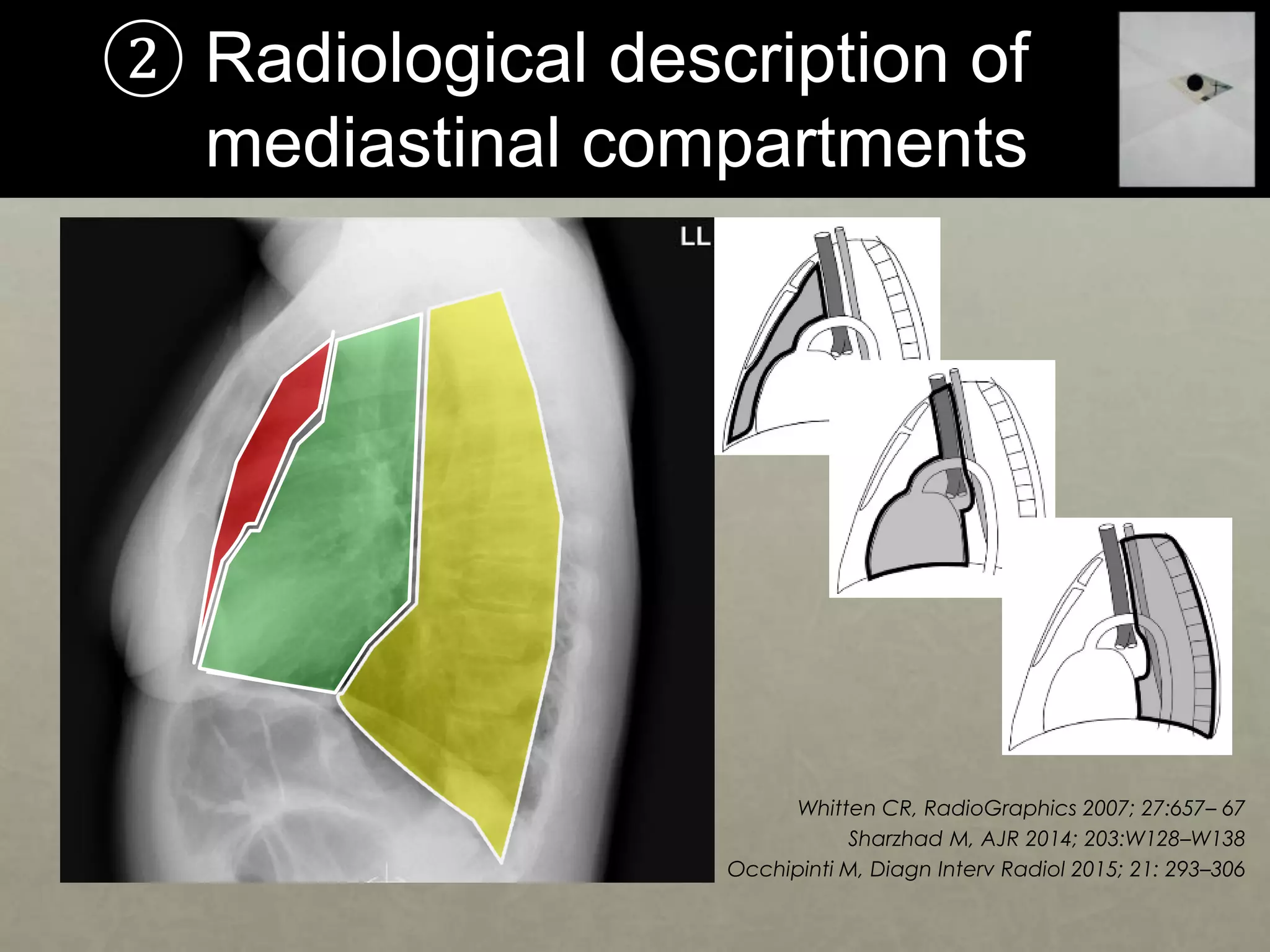
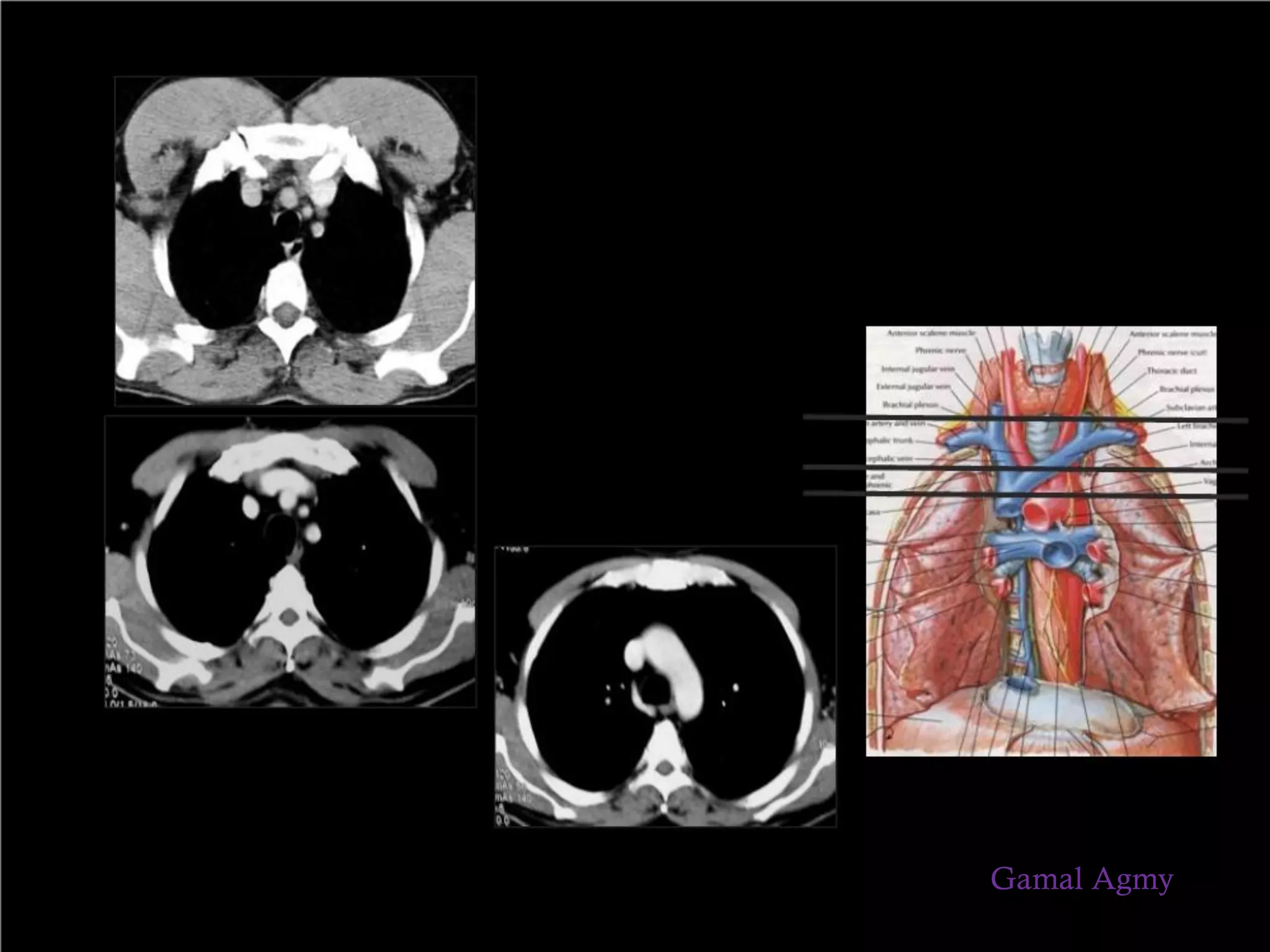
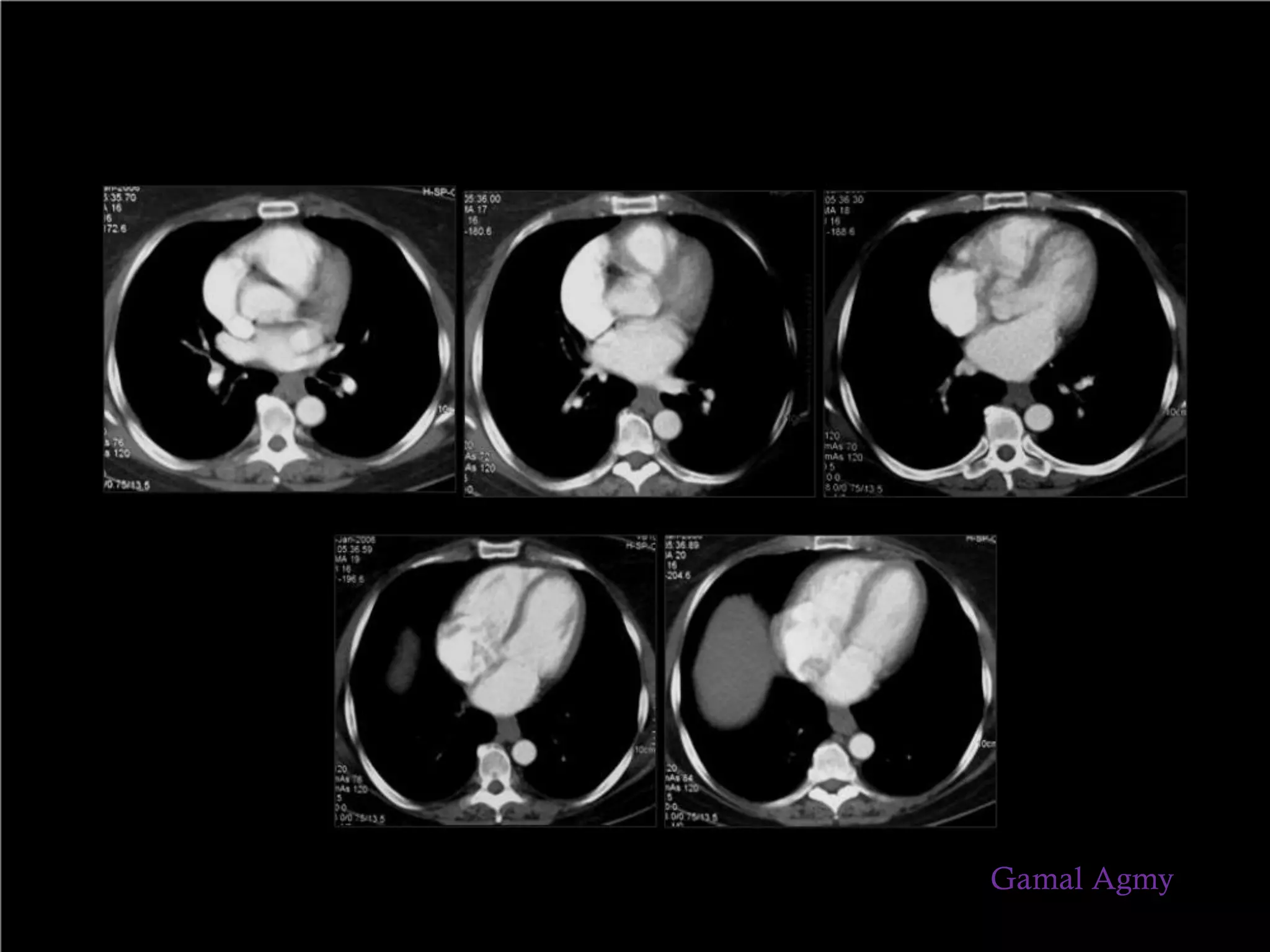
This document discusses the CT anatomy and imaging of the mediastinum. It outlines 6 objectives, including describing the CT anatomy of the mediastinum, pneumomediastinum, mediastinal lymphadenopathy, radiological description of mediastinal compartments, differential diagnosis of mediastinal disease, and interventional supply. It then provides detailed descriptions and images of the different mediastinal compartments and lymph node stations.








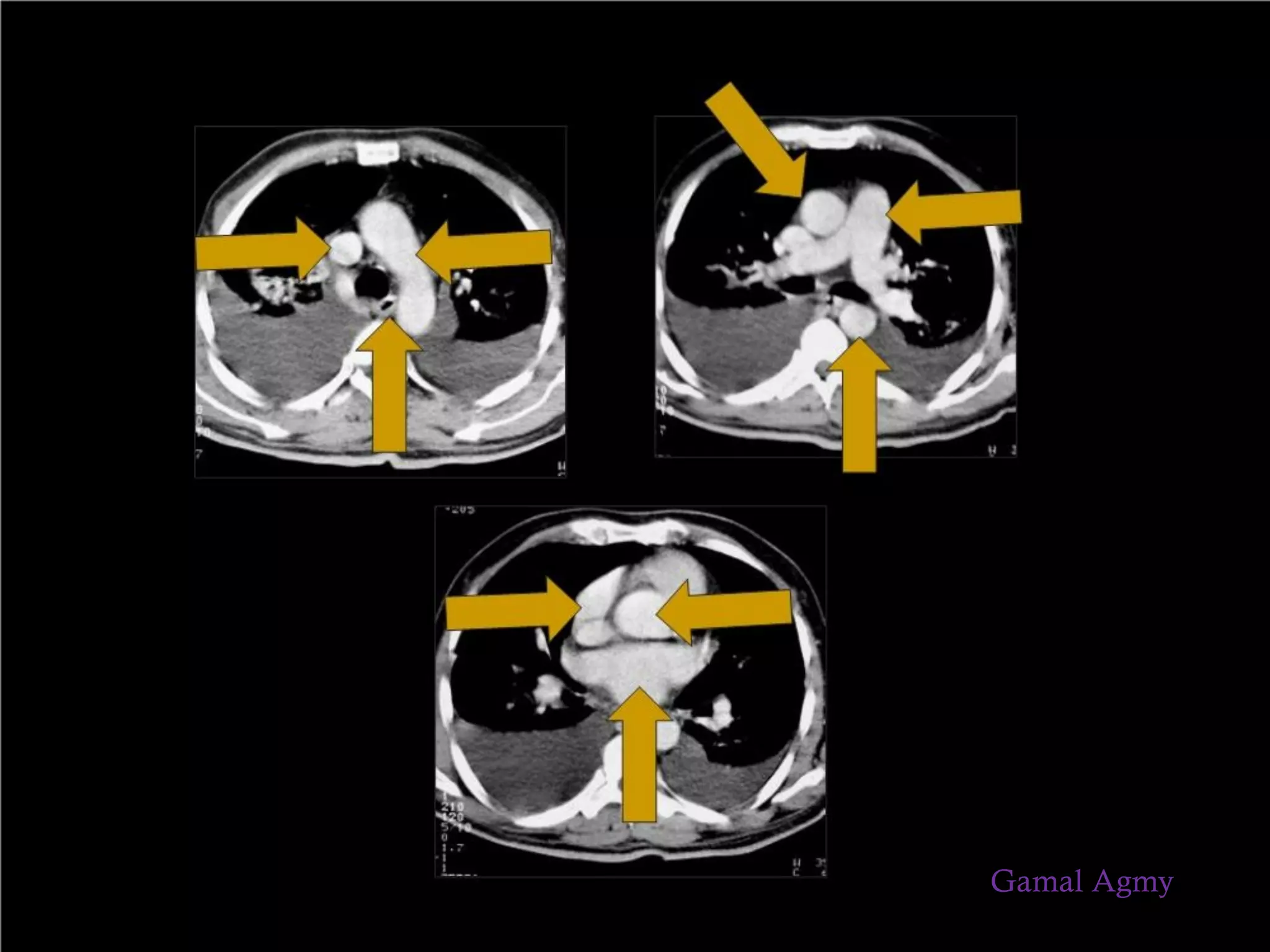










![Lymph
nodes
Nodes with necrotic center = inflammatory, metastatic
Bulky nodes = lymphoma
Calcifications seen in TB, sarcoid, silicosis
Calcification is rare in malignant nodes [chondro /
osteosarcoma]
General Rules
Gamal Agmy](https://image.slidesharecdn.com/imagingofmediastinum-180302202304/75/Imaging-of-Mediastinum-23-2048.jpg)