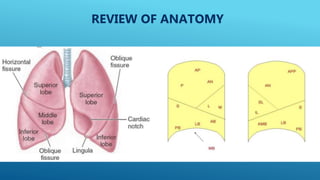
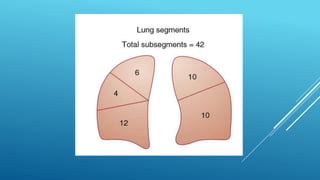
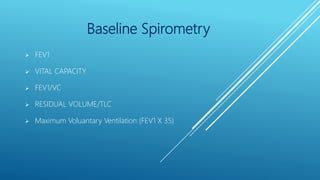
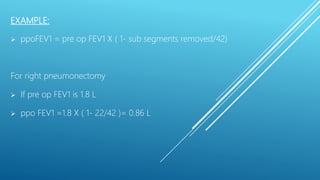
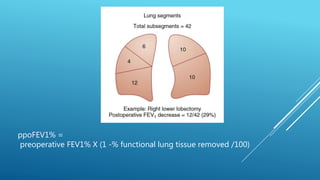
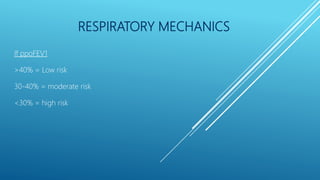
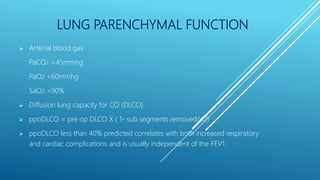
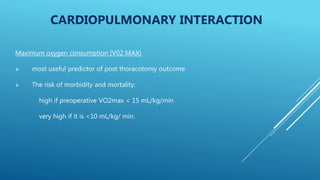
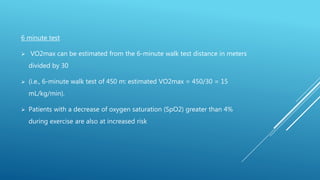
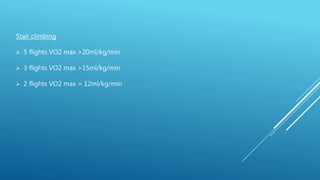
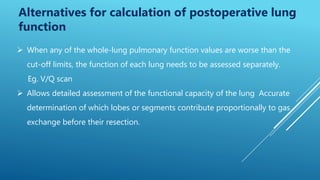
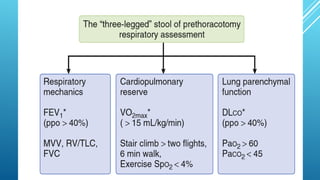
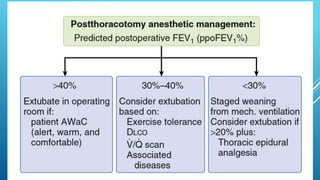
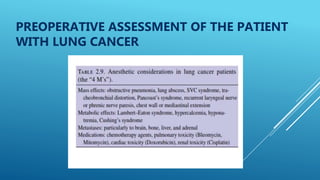
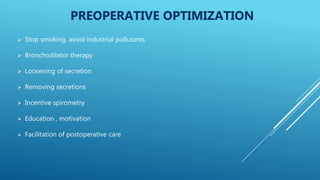
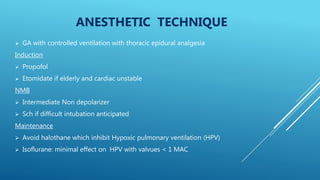
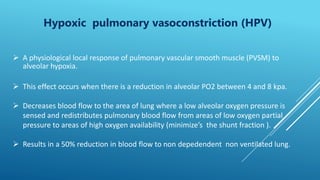
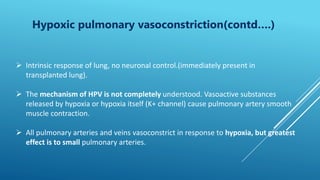
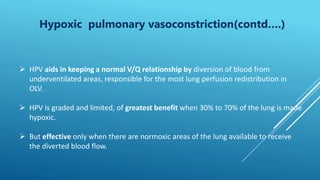
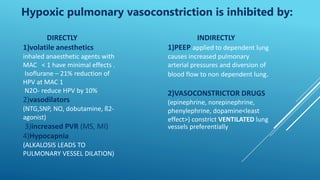
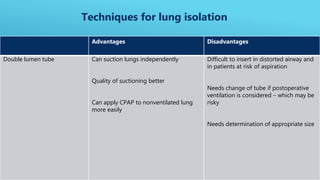
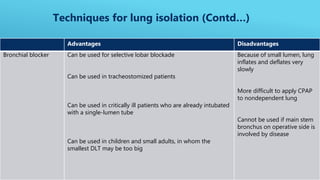
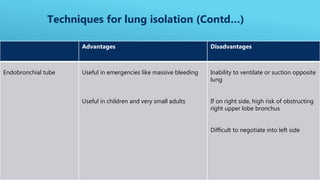
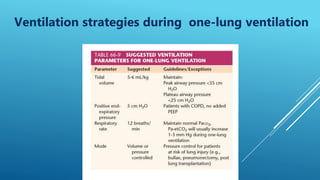
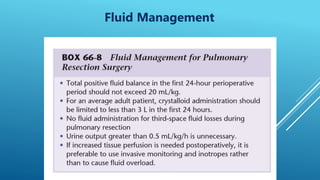
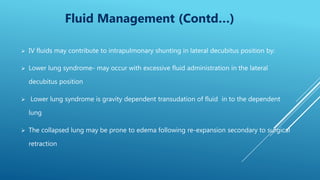
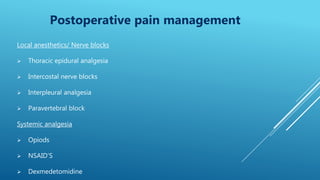
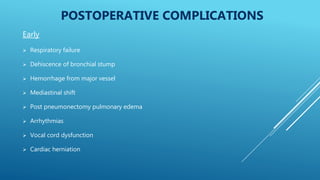
This document summarizes anesthesia considerations for pneumonectomy. It discusses pre-operative assessment of cardiopulmonary function to determine risk. Intra-operatively, techniques for lung isolation include double lumen tubes, bronchial blockers, or endobronchial tubes. Positioning is lateral, and one-lung ventilation requires strategies to manage hypoxemia. Post-operative monitoring and pain management involve thoracic epidural analgesia, intercostal blocks, and systemic opioids or NSAIDs to prevent complications like respiratory failure, hemorrhage, or pulmonary edema.