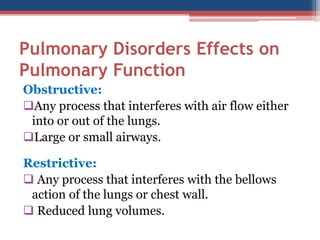
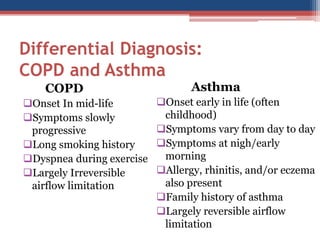
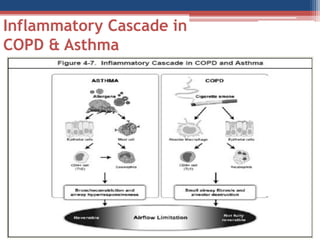
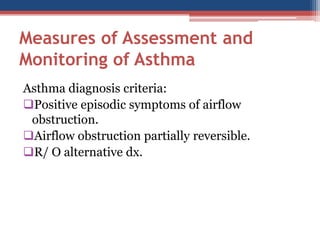
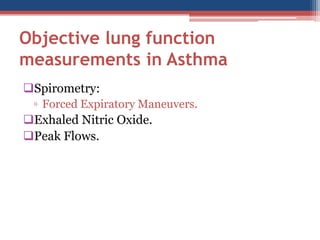
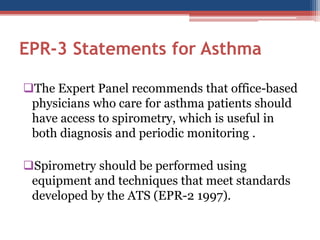
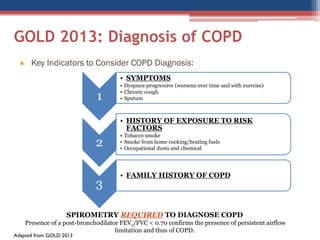
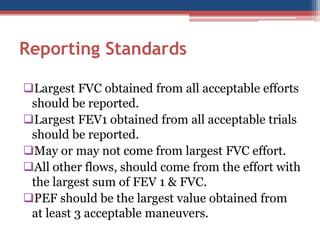
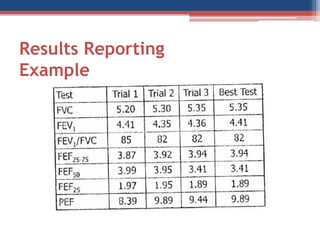
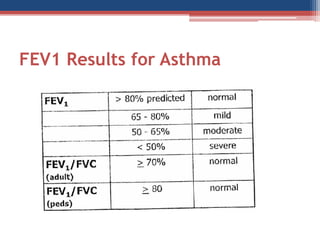
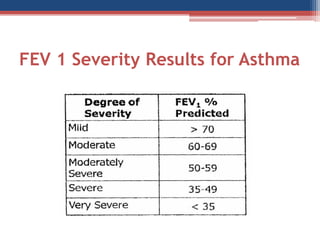
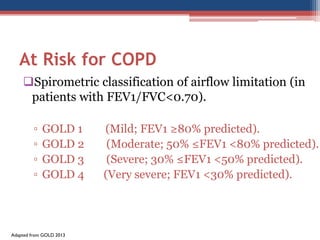
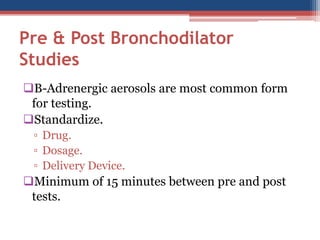
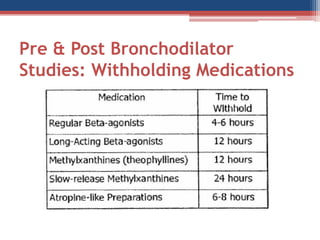
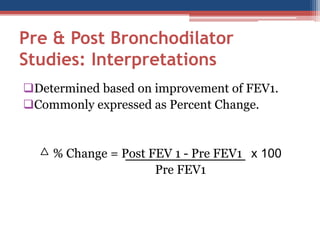
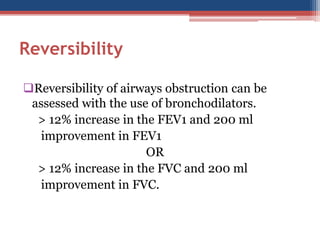
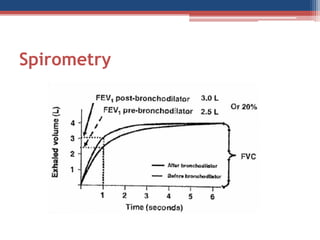
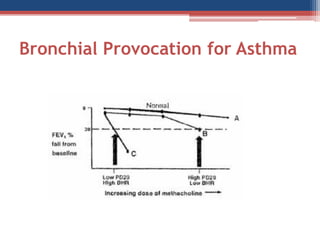
The document discusses spirometry as a crucial tool for diagnosing and monitoring obstructive lung diseases, particularly COPD and asthma. It outlines the differences between the two conditions, detailing symptoms, diagnostic criteria, and the importance of spirometry in assessing lung function and guiding treatment. The document further explains the testing procedures, interpretations of results, and the significance of understanding various spirometric measurements.