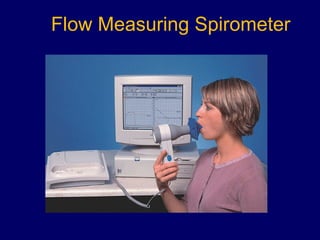
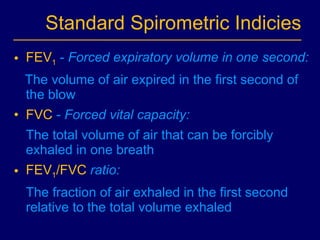
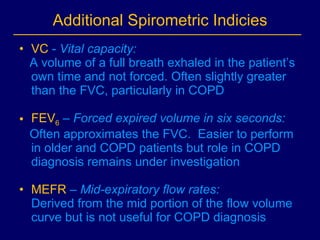
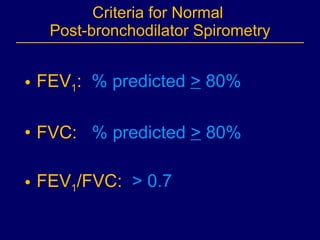
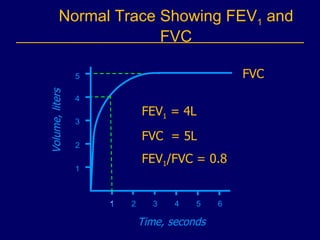
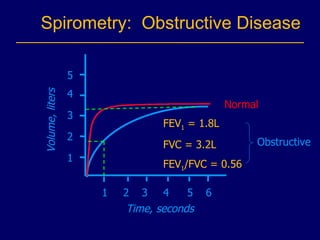
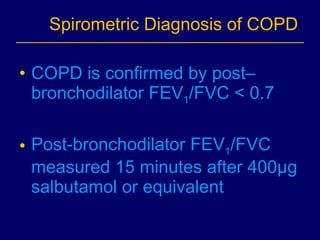
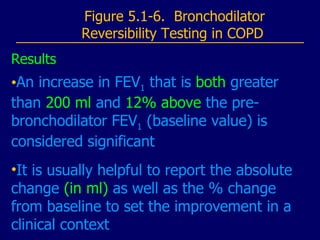
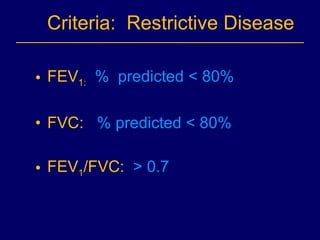
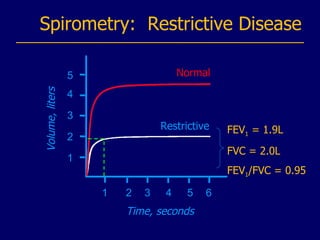
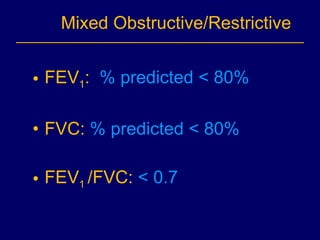
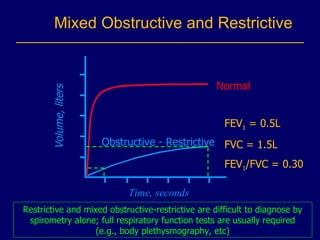
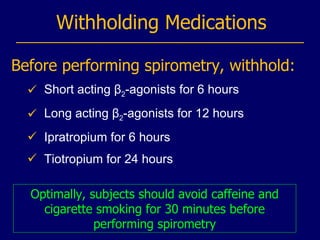
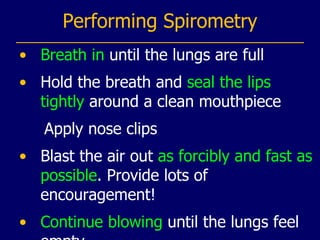
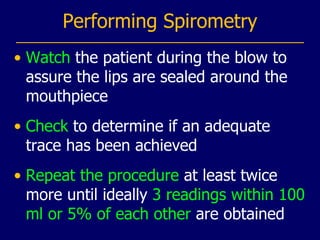
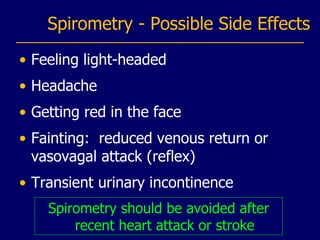
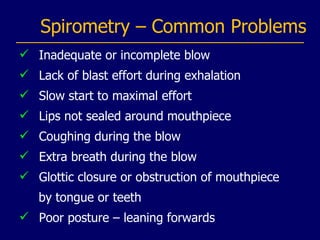
Spirometry is a test used to measure lung function by having a patient forcefully exhale into a spirometer. It measures volumes like forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) to diagnose and monitor conditions like COPD. The document discusses the different types of spirometers, normal values, how to interpret tests for obstructive, restrictive, and mixed lung disease patterns, and practical considerations for administering spirometry tests.